Br J Cancer:帕唑帕尼与拓扑替康联合治疗转移性和不可切除性软组织肉瘤患者的II期临床研究
2021-05-30 xiaozeng MedSci原创
软组织肉瘤 (STS) 是一种起源于间充质组织的罕见癌症。
软组织肉瘤 (STS) 是一种起源于间充质组织的罕见癌症。综合而言,所有肉瘤亚型约占成人癌症的1%。既往研究显示,大多数的转移性STS的一线治疗都涉及使用蒽环类药物的全身化疗(单独或联合治疗)。
血管生成是包括STS在内的恶性肿瘤生长的既定机制,肿瘤具有与血管化程度相关的转移潜力。虽然这是一个复杂的过程,但血管生成在很大程度上是由VEGF所驱动的。而VEGF通路可被酪氨酸激酶抑制剂(TKI)所抑制,如帕唑帕尼(pazopanib)。
最近的研究表明,帕唑帕尼对难治性软组织肉瘤(STS)有活性,可显著延长患者的PFS。因此,单独使用或与细胞毒性治疗联合使用或对肉瘤患者有效。
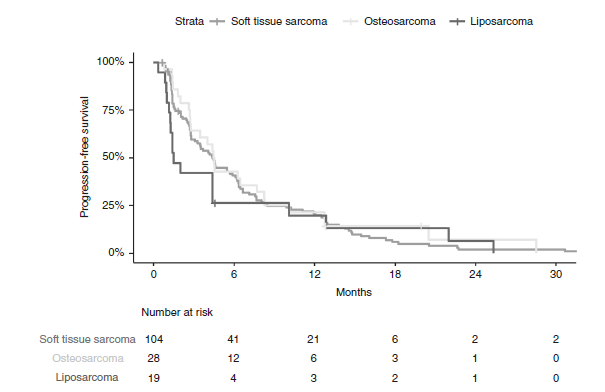
患者的无进展生存期
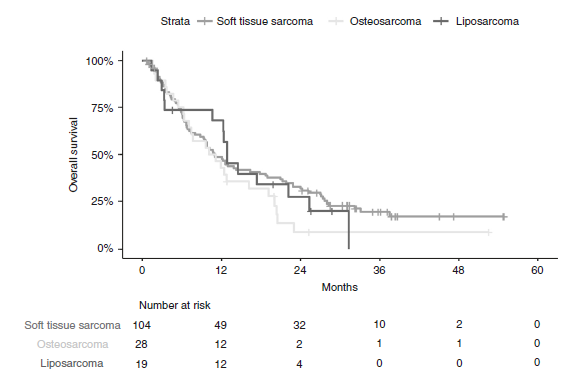
这项前瞻性、单臂、II期研究主要评估了帕唑帕尼与拓扑替康(topotecan)联合治疗转移性或不可切除性的非脂肪细胞瘤STS患者的疗效。此外,该试验还纳入了骨肉瘤和脂肪肉瘤的相关探索性研究。试验的主要终点是非脂肪细胞瘤STS队列中患者的12周无进展率。
患者的总生存率
结果显示,在该STS队列中,57.5%的患者在12周时表现为疾病的无进展,未达到研究的主要终点(66%)。探索性骨肉瘤队列研究则超过了先前建立的12%的II期试验比较数据基准,患者的12周PFR为69.55%。在大多数的患者中,帕唑帕尼和拓扑替康联合治疗伴有3或4级毒性。
总而言之,在这项前瞻性试验中,帕唑帕尼与拓扑替康的联合治疗并未达到其12周无进展率的主要终点。且帕唑帕尼与拓扑替康联合治疗与高度毒性相关。
原始出处:
Schulte, B., Mohindra, N., Milhem, M. et al. Phase II study of pazopanib with oral topotecan in patients with metastatic and non-resectable soft tissue and bone sarcomas. Br J Cancer (28 May 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








.jpg)




#II期临床研究#
29
#I期临床#
26
#联合治疗#
31
#转移性#
35
#软组织#
32
#II期临床#
37