2022年1月10日,联拓生物宣布,mavacamten在用于治疗有症状的梗阻性肥厚型心肌病(oHCM)的3期临床试验EXPLORER-CN中,完成了首位中国患者给药。
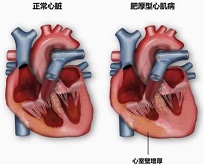
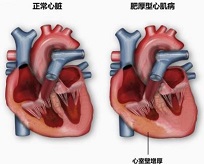
肥厚型心肌病是一种由心肌过度收缩和左心室血液充盈受阻引起的慢性进行性疾病,可导致衰弱症状和心脏功能障碍。据估算,全球每500人中就有1位肥厚性心肌病患者。肥厚性心肌病最常见的原因是心肌肌节蛋白的突变。在梗阻性或非梗阻性肥厚性心肌病患者中,劳力可导致疲劳或呼吸困难,影响患者的日常生活。肥厚性心肌病还与房颤、中风、心力衰竭和心源性猝死风险的增加有关。
“中国是世界上肥厚性心肌病患者最多的国家,预计约有超过100万中国患者,”联拓生物首席执行官王轶喆博士说。“在全球临床试验中,mavacamten显示出对肥厚性心肌病患者的治疗获益具有显著统计学意义和临床意义。联拓生物致力于加速这款具有潜在革新性和首创性的心肌肌球蛋白抑制剂的上市,并设计了关键的EXPLORER-CN临床试验,以支持其在中国的新药上市申请。”
EXPLORER-CN是一项多中心、双盲、随机、安慰剂对照的3期临床注册研究,旨在评估mavacamten在用于治疗有症状梗阻性肥厚型心肌病的中国患者中的疗效和安全性。EXPLORER-CN将招募约81位患者。其主要终点是用Valsalva左心室流出道(LVOT)梯度从基线到第30周的变化。符合条件的患者将继续接受长期延长治疗。

Mavacamten是一款潜在的首创、口服、心肌肌球蛋白别构调节剂,用于治疗以心肌过度收缩和心脏舒张充盈受损为内在原因的疾病。Mavacamten通过抑制过度的肌球蛋白-肌动蛋白横桥的形成来降低心肌收缩力,而过度的肌球蛋白-肌动蛋白横桥的形成可导致心肌收缩过度、左心室肥厚和顺应性降低。在临床和临床前研究中,mavacamten持续表现出降低心壁应力的生物标志物,减轻过度的心肌收缩、增加舒张顺应性。
用mavacamten治疗纽约心脏协会NYHA评级为II-III级的梗阻性肥厚性心肌病患者的全球3期临床试验EXPLORER-HCM的结果显示,mavacamten达到了所有主要和次要终点且具有显著的统计学意义,并证明其在功能状态、症状和生活质量方面的改善具有显著的临床意义。同时,联拓生物也正在进行mavacamten在中国健康志愿者中的药代动力学研究。该研究于2021年11月完成了患者给药。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#梗阻性肥厚型心肌病#
40
#3期临床#
50
#ACA#
28
#CAM#
46
#3期临床试验#
42
#肌病#
27