JTO: Durvalumab治疗同步放化疗后Ⅲ期EGFR突变的NSCLE患者研究结果
2021-05-27 MedSci原创 MedSci原创
2018年,度伐利尤单抗被美国食品和药物管理局批准作为同步放化疗(CRT)后III期非小细胞肺癌(NSCLC)患者的巩固免疫治疗。然而,度伐利尤单抗是否对EGFR突变的NSCLC患者有益仍不清楚。
2018年,度伐利尤单抗被美国食品和药物管理局批准作为同步放化疗(CRT)后III期非小细胞肺癌(NSCLC)患者的巩固免疫治疗。然而,度伐利尤单抗是否对EGFR突变的NSCLC患者有益仍不清楚。本研究主要对不可切除的EGFR突变的Ⅲ期NSCLC患者进行多机构回顾性分析,这些患者已经完成了CRT。利用Kaplan-Meier分析评估接受或不接受度伐利尤单抗的CRT患者的无进展生存期(PFS)。

在37名患者中,13名患者在完成CRT后中位数20天时开始使用度伐利尤单抗。其中,两名患者完成了12个月的治疗,五名患者因病情进展停用度伐利尤单抗,另五名患者因免疫相关不良事件(irAEs)而停用治疗。
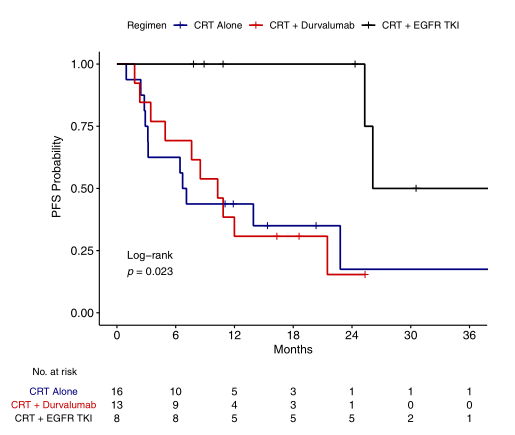
图1 不同组患者治疗的中位PFS
在24例完成CRT但未使用度伐利尤单抗的患者中,16例仅完成了CRT,8例患者完成CRT并使用诱导或巩固EGFR酪氨酸激酶抑制剂(TKIs)治疗。接受CRT和度伐利尤单抗治疗的患者中位PFS为10.3个月,而单独接受CRT治疗的患者中位PFS为6.9个月(log rank p=0.993)。与单独接受CRT或接受CRT联合度伐利尤单抗的患者相比,CRT联合EGFR TKI中位PFS显著延长(26.1个月)(log-rank p=0.023)。
在这项研究中,EGFR突变的NSCLC患者没有从度伐利尤单抗中受益,并可能更容易发生irAEs。在度伐利尤单抗治疗后使用奥希替尼的患者可能更容易发生irAEs。在这种情况下,应谨慎巩固使用度伐利尤单抗,诱导或巩固EGFR-TKIs联合CRT治疗可作为治疗方法。
Aredo, Jacqueline V. et al. Durvalumab for Stage III EGFR-Mutated NSCLC After Definitive Chemoradiotherapy. Journal of Thoracic Oncology, Volume 16, Issue 6, 1030 - 1041
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#mAb#
44
#研究结果#
31
#放化疗#
37
#同步放化疗#
34
#GFR#
33
学习了,谢谢分享
60