Eur Urol Focus:膀胱癌中机器人辅助与开放式膀胱癌根治术的比较
2021-07-12 AlexYang MedSci原创
开放式根治性膀胱切除术(ORC)是肌层浸润性膀胱癌的标准治疗方法,但机器人辅助根治性膀胱切除术(RARC)在实践中的应用越来越多。最近的一项研究显示,RARC导致的轻微并发症略少,但主要并发症略多,但
开放式根治性膀胱切除术(ORC)是肌层浸润性膀胱癌的标准治疗方法,但机器人辅助根治性膀胱切除术(RARC)在实践中的应用越来越多。最近的一项研究显示,RARC导致的轻微并发症略少,但主要并发症略多,但这种差异没有统计学显著意义。在次要结果中发现了一些有利于RARC或ORC的差异。研究人员预计RARC的使用在未来几年会增加,从而促进了关于RARC是否更经济的争论。

近期,有研究人员评估了RARC与ORC在膀胱癌治疗中的经济效益情况。
该项经济评估是与一项前瞻性的多中心有效性比较研究同时进行的。研究人员纳入了来自19家荷兰医院的348名膀胱癌患者(ORC,n=168;RARC,n=180)。在1年内,研究人员从医疗和社会的角度评估了每个质量调整生命年(QALY)的增量成本。
结果表明,每位患者的平均医疗费用为:ORC为17141欧元(95%置信区间[CI]为15791-18720欧元),RARC为21266欧元(95% CI为19163-23650欧元)。每位患者的平均社会成本:ORC为18926欧元(95% CI为17431-22642欧元),RARC为24896欧元(95%CI为21925-31888欧元)。平均而言,RARC患者获得了0.79个QALYs(95%CI 0.74-0.85),而ORC患者获得了0.81个QALYs(95%CI 0.77-0.85),平均QALY差异为-0.02(95%CI -0.05 至 0.02)。使用8万欧元的成本效益阈值,从医疗和社会角度,RARC分别在0.6%和0.2%的重复中具有经济效益性。
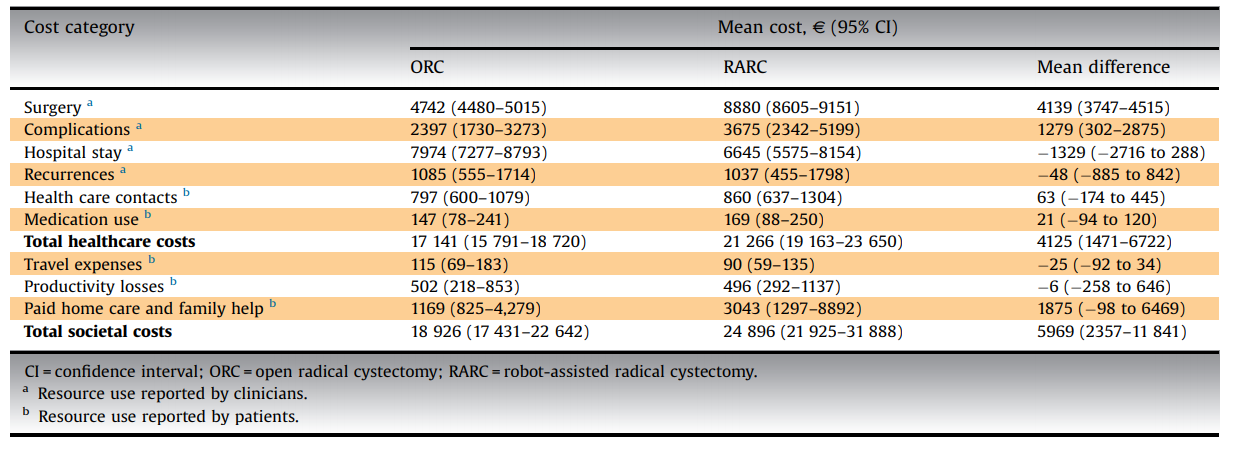
1年随访期间每位患者ORC和RARC的医疗和社会平均花费
综上所述,RARC在QALYs方面没有显示出优越性,但比ORC更昂贵。因此,与ORC相比,RARC似乎并不划算。
原始出处:
Charlotte T J Michels, Carl J Wijburg, Gerjon Hannink et al. Robot-assisted Versus Open Radical Cystectomy in Bladder Cancer: An Economic Evaluation Alongside a Multicentre Comparative Effectiveness Study. Eur Urol Focus. Jun 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












已读
58
#机器人#
18
#根治术#
29
#机器人辅助#
46
#机器#
21
#根治#
23
学习
55
膀胱癌真怪,明明是免疫敏感性肿瘤,为什么PD-1治疗效果不好呢?难道靶点不对?将来CD47会不会有效
47
放式根治性膀胱切除术(ORC)是肌层浸润性膀胱癌的标准治疗方法。
47