JAMA Netw Open:先天性心脏病患儿手术治疗后患高血压的长期风险是普通儿童的12倍!
2021-04-10 Nebula MedSci原创
先天性心脏病患儿手术治疗后患高血压的长期风险是普通儿童的12倍!
先天性心脏病(CHD)是最常见的先天性缺陷,在美国约有240万CHD患者。尽管许多CHD患儿无需手术干预,但约有四分之一的CHD患儿需要心脏手术治疗。
但是,迄今为止,CHD治疗术后患儿高血压的长期风险尚不清楚。该研究旨在了解CHD患儿心脏手术后高血压的发生率。
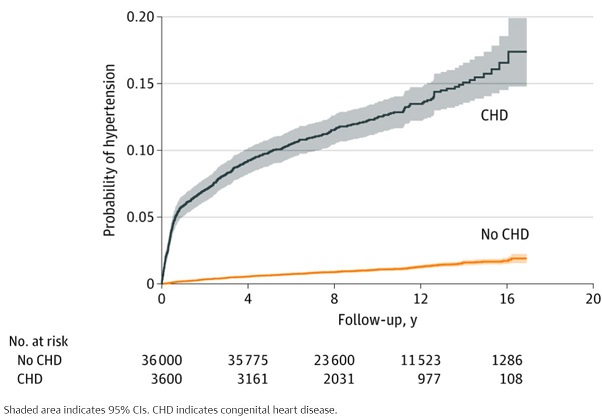
这是一项在加拿大开展的多中心回顾性配对队列研究。通过检索数据库,共纳入了3600名接受手术修复CHD的患儿,以及在年龄、性别、指标日期、农村地区和社区收入方面相匹配的来自普通人群的36000名无CHD的儿童。主要评估指标是术后中位随访9.8年内高血压的发生率。最后一次随访时间是2019年3月31日。
高血压的发生率
总体而言,在3600名接受CHD外科修复的患儿(2005名男孩)中,首次手术的平均年龄为150天(四分位数范围为 40-252天)。随访期间,445名(12.4%)的经手术修复CHD的患儿罹患高血压,相比之下,匹配的对照组中仅有398名(1.1%)儿童出现了高血压(P<0.05)。CHD手术组儿童高血压的发病率为141.3(95%CI,128.8~155.1)/10000人·年,而对照组为11.1(95%CI,10.1~12.3)/10000人·年。
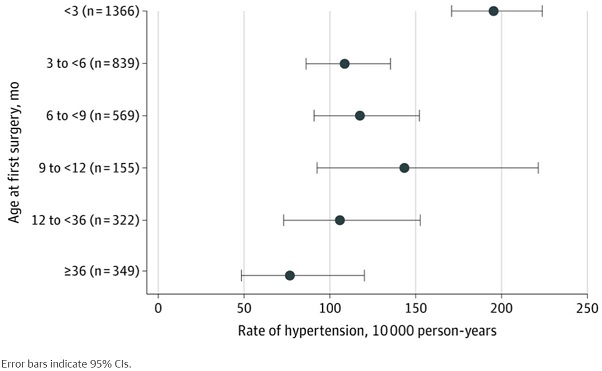
手术治疗时的年龄对高血压风险的影响
与那些在150天或更大年龄时进行手术的儿童相比,在不足150天大时进行手术的儿童患高血压的风险更高(P=0.006)。在心脏外科住院期间,接受的手术越复杂,特别是左心发育不良综合征患儿(49/140[35.0%])和接受透析的患儿(22/126[17.5%];危险比 1.67;95%CI 1.09-2.56),患高血压的风险越高。
总之,该研究显示,接受CHD手术治疗的儿童的长期高血压发病率是基本情况相匹配的无CHD的儿童的12倍,提示:这类患儿人群需要旨在降低心脏手术后高血压长期风险的干预措施。
原始出处:
Greenberg Jason H,McArthur Eric,Thiessen-Philbrook Heather et al. Long-term Risk of Hypertension After Surgical Repair of Congenital Heart Disease in Children. JAMA Netw Open, 2021, 4: e215237.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#NET#
45
#PE#
36
#手术治疗#
40
#先天性#
44
#长期风险#
42
好
82
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
58