Hepatology:与单纯HCV感染者相比,HIV/HCV感染的肝硬化患者不再具有更高的肝癌或晚期肝病风险
2019-02-01 李娜 胡玉琳 临床肝胆病杂志
HIV感染被普遍认为是HCV患者肝病加重的一个危险因素。然而,由于cART具有更好的疗效和安全性,使丙型肝炎患者获得治疗的机会增加,这种情况是否仍然存在尚不清楚。
HIV感染被普遍认为是HCV患者肝病加重的一个危险因素。然而,由于cART具有更好的疗效和安全性,使丙型肝炎患者获得治疗的机会增加,这种情况是否仍然存在尚不清楚。
1253例单纯HCV患者和175例HIV/HCV患者被纳入2组前瞻性法国国家队列研究(ANRS CO12 CirVir和CO13 HEPAVIH)。纳入标准为代偿期肝硬化(Child‐Pugh A),无既往并发症史,并进行了肝活组织检查评估。肝硬化失代偿发生率、肝癌的发生率和死亡率根据HIV状态由Fine-Gray模型调整年龄后计算。倾向得分匹配法根据基线特征将混杂变量的影响最小化。
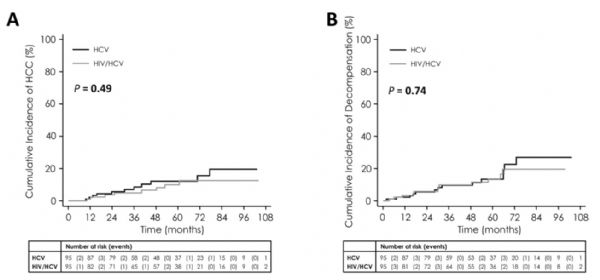
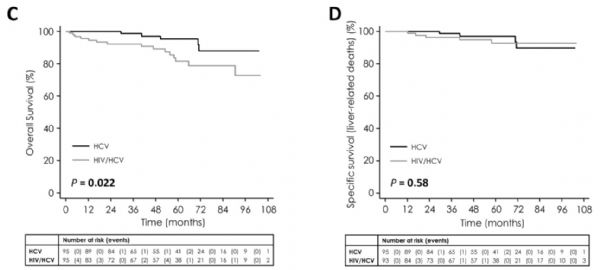
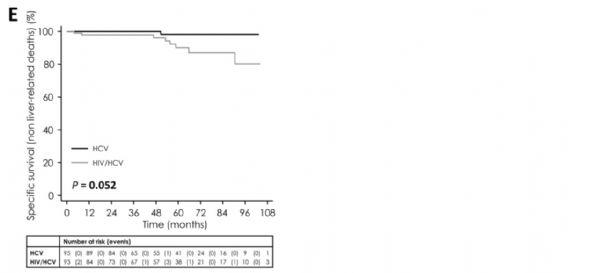
在基线水平,HIV/HCV患者较年轻(47.5岁 vs 56.0岁,P<0.001),男性多于女性(77.1% vs 62.3%,P<0.001)。在基线水平及随访结束时,HCV的根除率与单纯HCV患者相似。80.4% HIV/HCV患者携带检测不到的HIV病毒载量。年龄调整后,HIV/HCV与HCV患者的5年累积肝癌和失代偿发生率相似。HIV/ HCV患者经年龄调整后的总死亡率更高(SHR=1.88, 95%CI: 1.15~3.06, P=0.011)。年龄、SVR的缺失、肝硬化的严重程度是影响肝硬化失代偿和肝癌的相关因素,但与HIV状态无关。根据基线特征对每组95例患者进行倾向性评分,观察到了相似的结果。
在HCV感染的肝硬化患者中,合并HIV感染不再与更高的肝癌和肝失代偿风险相关。然而,存在肝外疾病时死亡率会持续上升。
原始出处:D Salmon‐Ceron, Pierre Nahon, Richard Layese, et al. HIV/HCV co‐infected cirrhotic patients are no longer at higher risk for HCC or end‐stage liver disease as compared to HCV mono‐infected patients. Hepatology. 19 December 2018
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#晚期肝病#
30
#HCV#
27
#EPA#
30
#HCV感染#
35
学习
75
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
82
谢谢!最新的信息读起来就是收获大
54