JAHA:COVID-19住院3个月后的心脏功能障碍和心律失常负担
2022-01-24 MedSci原创 MedSci原创
COVID-19出院3个月后,右心室功能轻度受损,舒张功能障碍的发生率是对照组的两倍。几乎没有证据表明心脏功能与重症监护治疗、呼吸困难或疲劳之间存在关联。
COVID-19后心功能不全的严重程度各不相同,并且缺乏关于心律失常负担的数据。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,这是一项联合多中心前瞻性队列研究和横断面病例对照研究。研究人员将出院后3至4个月的COVID-19患者通过超声心动图评估的心脏功能并与匹配的对照组进行比较。
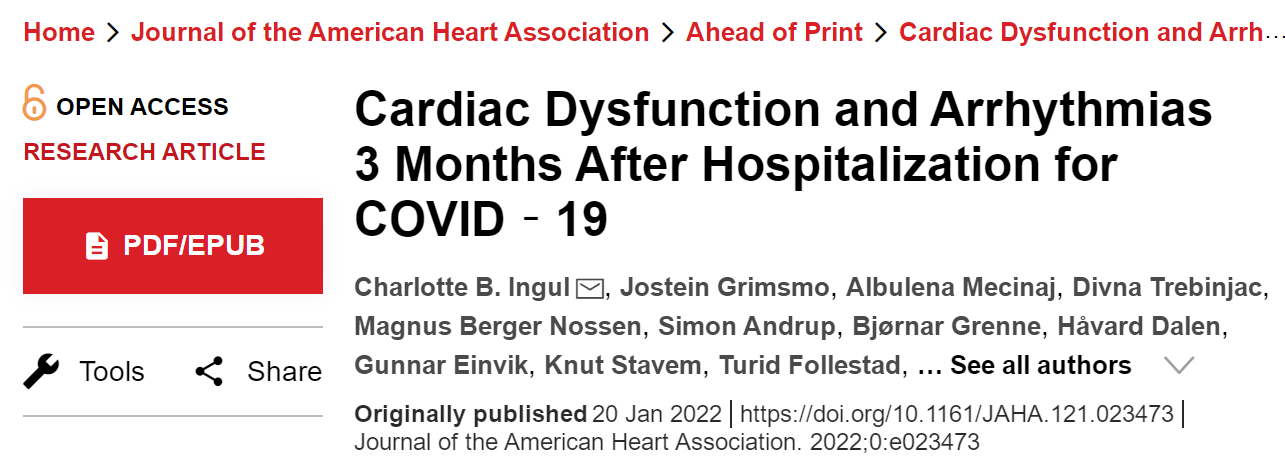
研究人员记录了COVID-19患者的24小时心电图数据。该研究共有204名COVID-19患者同意参与试验(平均年龄为58.5岁;44%为女性),以及204名对照者(平均年龄为58.4岁;44%为女性)。
与对照组相比,COVID-19患者右心室游离壁纵向应变更严重(调整后的估计平均差为1.5个百分点;95%CI为-2.6至-0.5;P=0.005)和三尖瓣环平面收缩期偏移(-0.10cm;95%CI为-0.14至-0.05;P<0.001)和心脏指数(-0.26L/min/m2;95%CI为-0.40至-0.12;P<0.001)较低,但左心室整体应变稍好(-0.8个百分点;95%CI为0.2-1.3;P=0.008)。与对照组相比,舒张功能下降的发生率是对照组的两倍(分别为60[30%] vs. 29[15%];比值比为2.4;P=0.001)。呼吸困难或疲劳与心脏功能无关。重症监护治疗后右心室游离壁纵向应变更严重。27%的患者出现心律失常,主要包括室性早搏和非持续性室性心动过速(分别为18%和5%)。
由此可见,COVID-19出院3个月后,右心室功能轻度受损,舒张功能障碍的发生率是对照组的两倍。几乎没有证据表明心脏功能与重症监护治疗、呼吸困难或疲劳之间存在关联。室性心律失常很常见,但其临床重要性尚未明确。
原始出处:
Charlotte B. Ingul.et al.Cardiac Dysfunction and Arrhythmias 3 Months After Hospitalization for COVID‐19.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.023473
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











很不错的研究发现,学习了,非常感谢
53
#心脏功能障碍#
37
#AHA#
39
#心脏功能#
68
#功能障碍#
38