ESMO OPEN:COVID-19背景下肿瘤学临床试验的新操作方法和地理差异
2021-12-28 MedSci原创 MedSci原创
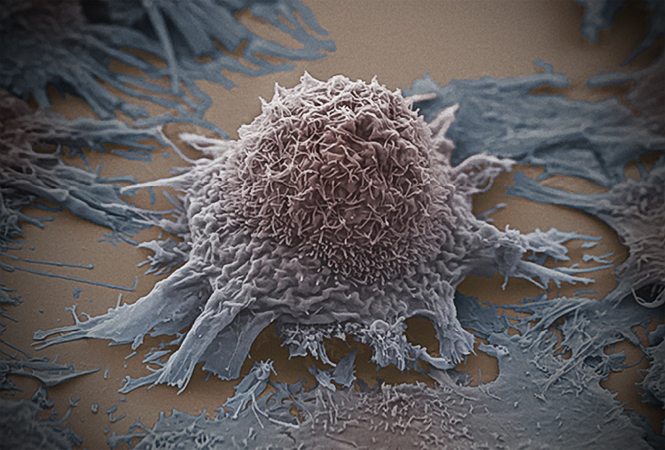
大流行对不同地区和国家的癌症患者治疗和肿瘤临床试验产生了各种影响。与某些癌症相关的高死亡率肯定促使患者和医生继续进行持续治疗。但是,存在非紧急医疗问题的患者不允许进入一些医疗保健机构。随着人们
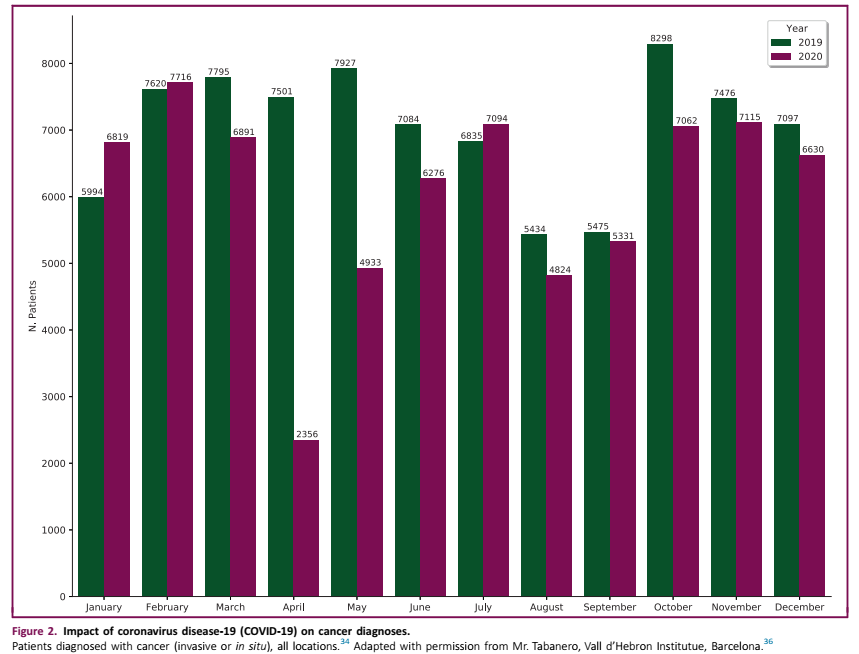
大流行对不同地区和国家的癌症患者治疗和肿瘤临床试验产生了各种影响(图1)。与某些癌症相关的高死亡率肯定促使患者和医生继续进行持续治疗。但是,存在非紧急医疗问题的患者不允许进入一些医疗保健机构。随着人们推迟筛查程序,新的癌症诊断减少;这可能在不久的将来导致晚期诊断增加(图2)。

在大流行期间,各机构旨在通过最小化和精简单位流动优化意义上的程序,并以远程选择取代当面访视,限制患者在其场所花费的时间。虽然这些手术旨在降低COVID感染的风险,但也有效降低了患者的护理和临床试验负担。
从操作角度优化试验设计和研究实施,更精简的临床访视以及在患者家中进行的一些访视和治疗,可以减少参与临床试验的负担,同时将试验的覆盖范围扩大到更广泛的人群(表1)。
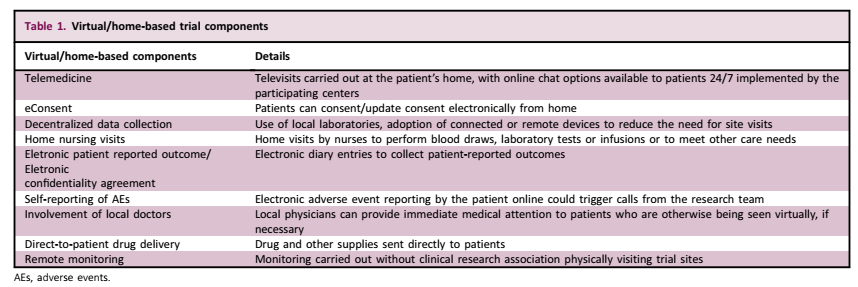
虚拟方法包括通过远程医疗和远程设备进行远程评估,并得到结构化数据收集的支持,使用靠近患者居住地点的实验室和成像设施进行分散的数据收集。它们还包括采用连接器械、家庭护理访视和直接向患者运送药物。
同样,已经推广和实施了远程监测,伴或不伴集中监测和基于风险的方法,以取代现场监测,监管机构之间在试验类型和持续时间方面也存在差异。临床试验利益相关者之间的合作可以推进创新,重点是验证和接受虚拟和混合试验的以下部分:
1. 肿瘤学研究的类型可以受益于新的操作方法
根据IQVIA的经验,大多数肿瘤学临床试验可以从混合方法而不是完全虚拟的解决方案中获益。后者更适用于长期随访研究等非干预性研究。是否采用新的操作方法,要根据以下因素对每项研究进行评估:研究分期(例如,早期与晚期阶段)、试验药物或干预的作用方式、给药途径(例如,口服与静脉给药)、安全性和耐受性特征、患者人群以及研究目的和终点。
2. 远程医疗实施的地理和文化差异
远程技术(包括远程医疗)采用的地理差异正在影响当地采用新的业务方法,并可能危及研究中心参与分散的试验。
在意大利,医生和患者之间的远程医疗目前主要涉及电话和电子邮件,而医生到医生的咨询包括放射学图像的共享,如计算机断层扫描,以及实验室结果。然而,意大利的肿瘤学家对将远程医疗直接用于患者持保留意见,原因是相信成功的肿瘤治疗需要建立医生和患者之间的个人关系,这可能很难远程创建。远程医疗仅由意大利肿瘤学家支持用于沟通实验室结果。
在亚洲国家,目前远程医疗主要在临床试验之外使用。患者通常喜欢选择通过电话或视频与医生沟通,并减少旅行需求。当地肿瘤学家建议,只有当新的医疗信息例如来自血液检测或成像的沟通,需要医疗咨询时,才应支付远程医疗的费用。
在美国,医疗许可证是按州颁发的,因此限制了在国内跨州边界提供远程医疗的能力。这限制了患者接触医生和他们可能接触到的试验。
来自欧洲患者社区(黑色素瘤患者网络欧洲)对远程医疗的反应好坏参半。例如一些患者担心错过了与他们的治疗肿瘤学家的现实世界互动。另一些同样情况的人却发现,能够有家庭成员陪伴是有益的。由于差旅费和自付费用(如停车费)减少,患者认为对其生活的影响显著降低。患者赞赏预定的互动,而不是超负荷的咨询或广泛的回调窗。
3. 采用远程监测的地理差异
远程监测依赖于适当技术的可用性和使用私人患者数据的授权。当地和地区差异可能对研究者和研究中心参与试验产生强烈影响。
解决机密性和数据安全的地区差异可能会为申办方和监查员制定各种规则,增加复杂性和成本。
在瑞士,由于数据保护问题,以及医院不允许从防火墙外访问患者病历的事实,目前无法进行远程监测。此外,访问将是全或无的,没有选项只提供对图表中定义的元素的访问。瑞士临床癌症研究小组(SAKK)报告称,国家监管机构Swissmedic正在允许大流行期间临床试验的微小变化。
在意大利,目前很少有机构(估计65家意大利临床研究中心中有2家)允许远程监测或提供电子健康记录(EHR)的访问。这是由于担心患者隐私,研究中心的EHR可用性不如其他国家广泛,缺乏能够选择性共享与给定临床试验相关的EHR要素的可用技术。国家正在努力创建肿瘤EHR网络。
在西班牙,监管机构允许对COVID-19试验和肿瘤学试验进行远程监测。机构之间以及制药公司和临床研究组织(CRO)之间的实施率不同。
在美国,大流行期间,远程监测迅速成为许多地点的常态。但是,一些研究中心发现这种方法比其他研究中心更难使用,因为需要签署严格的合同,以尽量减少违反患者机密性的可能性。
原文链接:https://pubmed.ncbi.nlm.nih.gov/34953404/
The impact of COVID-19 on cancer care and oncology clinical research: an experts’ perspective
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



.jpg)






#地理差异#
26
#PE#
34
#SMO#
27
#ESMO#
28
#肿瘤学#
0