Nature:诺奖得主全新发现,生物体竟会通过挤压来清除癌细胞,为癌症治疗带来新思路
2021-05-12 “E药世界”微信号 “E药世界”微信号
2021年5月5日,诺奖得主、麻省理工学院 Robert Horvitz 教授团队在 Nature 期刊发表了题为:Replication stress promotes cell eliminati
对于所有动物而言,清除某些细胞是胚胎发育中所必须的,活细胞在成熟组织中也会自然脱落。例如,肠壁每隔几天就会完全焕新一次。
生物体清除不需要的细胞的一种方式是通过称为细胞挤压的过程,该过程将细胞从组织层中挤出,而不会破坏留下的细胞层。 这一过程之前就已经被观察到,但生物体如何触发这一过程,仍然是个谜。
2021年5月5日,诺奖得主、麻省理工学院 Robert Horvitz 教授团队在 Nature 期刊发表了题为:Replication stress promotes cell elimination by extrusion 的研究论文。
研究人员在线虫中发现,当细胞分裂过程中细胞无法复制其DNA时,就会触发细胞挤压的过程。并进一步表明,哺乳动物细胞可以驱动相同的过程。
细胞挤压是从海绵到昆虫再到人类等生物体都在使用的细胞清除机制,这种机制可能是生物体清除癌细胞或癌前细胞的一种方式,为癌症治疗带来一种全新的思路。
细胞凋亡
在19世纪80年代,Robert Horvitz 教授就开始了对一种名为凋亡(apoptosis)的程序性细胞死亡进行研究,生物体通过凋亡来清除自己不再需要的细胞。
Robert Horvitz 教授使用秀丽杆线虫线虫(C. elegans)进行研究,这种仅有1毫米长的透明小虫是一种著名的模式动物,它的每个细胞的发育谱系都是已知的,并且每次胚胎发育都遵循相同的模式。在整个发育过程中产生了1090个细胞,并通过凋亡杀死其中的131个细胞,最终形成一个仅包含959个细胞的个体。
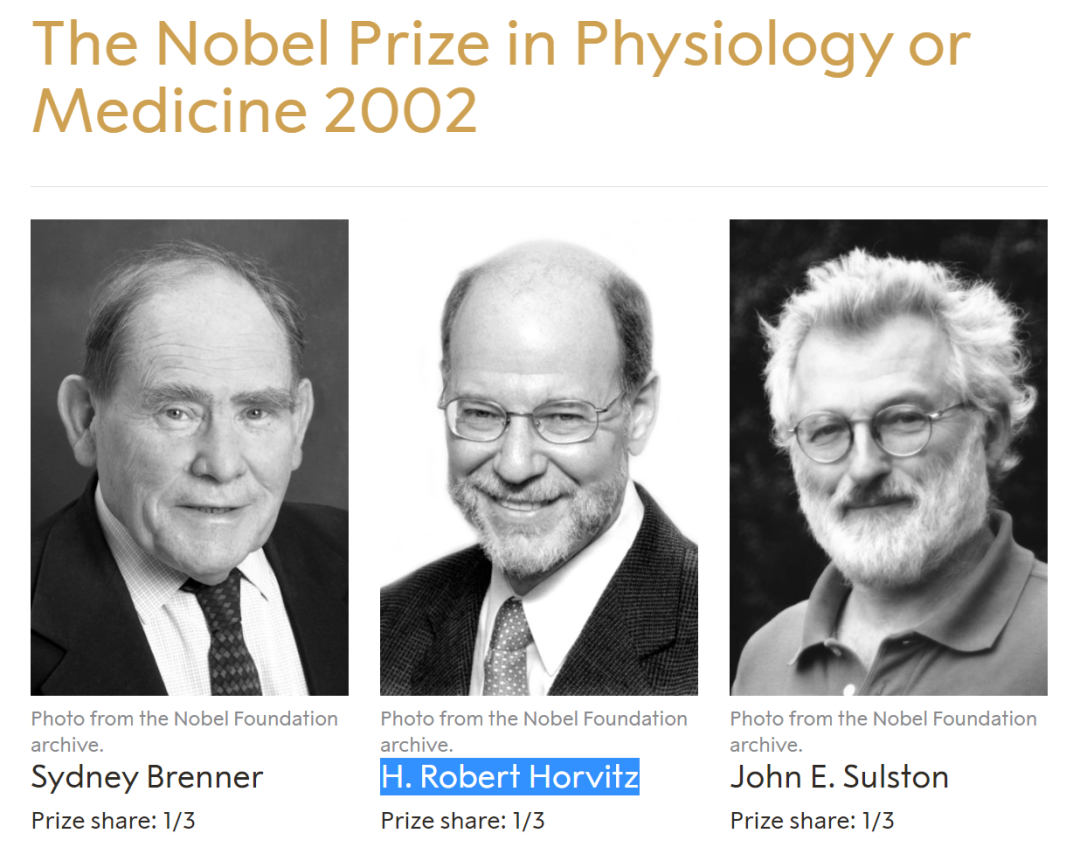
2002年,Robert Horvitz、Sydney Brenner、John Sulston 三人因发现器官发育和细胞程序性死亡的遗传调控机理而荣获当年的诺贝尔生理学或医学奖。
后来,Robert Horvitz 教授团队发现,如果线虫经过基因突变后无法通过凋亡来清除细胞,那么这131个细胞中的少数将通过细胞挤压清除,这种细胞挤压似乎可以作为细胞凋亡的备用机制。
但是,如何触发这一细胞挤压过程仍然是一个谜。
陷入细胞周期
为了揭开这个谜底,研究团队进行了大规模基因筛选,共筛选了超过11000个秀丽隐杆线虫基因。研究团队逐个敲低了无法执行细胞凋亡的线虫中的每个基因的表达,通过这种筛选,能够鉴定出对于发育过程中开启细胞挤压至关重要的基因。
令人惊讶的是,许多在细胞挤压过程中必不可少的基因同时参与细胞分裂周期。这些基因在细胞周期的最初阶段活跃,启动细胞分裂周期并复制细胞DNA。
进一步的实验表明,最终被挤出去的细胞确实开始进入细胞周期并开始复制其DNA。但是,它们似乎在此阶段被卡住,无法继续分裂,导致它们被其他细胞挤出。
大多数最终被挤出的细胞都异常小,它们是由不平等的细胞分裂产生的,导致一个大的子细胞和一个小得多的子细胞。研究团队发现,如果干扰了控制该过程的基因,从而使两个子细胞大小接近,那么原本应该被挤出的细胞就能够成功完成细胞周期,而不会被挤出。

中间红色的细胞正在被从线虫胚胎组织中挤出去
研究团队还发现,这种异常小的细胞无法完成细胞周期的原因是复制DNA时所需的蛋白质和DNA组分。在其他关键蛋白质中,这些细胞可能没有足够的LRR-1酶,这对DNA复制至关重要。
当DNA复制停止时,负责检测复制压力的蛋白质会使CDK1蛋白失活,从而迅速停止细胞分裂。此外,CDK1还有一个重要功能,就是控制细胞粘附,因此研究团队推测,当CDK1蛋白失活时,细胞会失去粘性并脱落,从而导致被挤出。
癌症保护
接下来,研究团队开始研究哺乳动物细胞是否可能有相同的细胞挤压。结果发现,在哺乳动物中,细胞挤压在替换肠、肺和其他器官的内壁细胞中起着重要作用。
研究团队使用一种叫做羟基脲的化学物质来诱导培养皿中生长的犬肾细胞的DNA复制压力,结果发现,这种处理使细胞挤出速率提高了三倍。
该研究还发现,在哺乳动物细胞中,众所周知的癌症抑制因子p53参与启动经历复制压力的细胞的挤出。这表明p53除了具有已知的癌症保护作用外,还可以通过挤出癌变细胞或癌前细胞来起到保护作用。
复制压力是癌前细胞或癌变细胞的特征之一,这些发现表明,挤出受到复制压力的细胞可能是一种抑癌机制。
从低等的海绵,到高等的哺乳动物,都可以观察到存在细胞挤压,而且,这种通过细胞挤压来清除细胞的机制只依赖细胞周期,不需要像细胞凋亡那样需要专门的机制来执行。因此研究团队推测它可能是一种非常早期的细胞清除形式,后来被涉及细胞凋亡的程序性细胞死亡所取代。
总的来说,该研究发现了当细胞分裂过程中细胞无法复制其DNA时,就会触发细胞挤压的过程,并证实了这一机制在动物中广泛存在,这种机制可能是生物体清除癌细胞或癌前细胞的一种原始方式,为癌症治疗带来一种全新的思路。
原始出处:
Dwivedi, V.K., Pardo-Pastor, C., Droste, R. et al. Replication stress promotes cell elimination by extrusion. Nature (2021). https://doi.org/10.1038/s41586-021-03526-y.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新发现#
33
#癌症治疗#
43
#Nat#
28
#新思路#
38
#癌细胞#
33
#诺奖#
30