NEJM:Bimekizumab VS. Secukinumab 治疗斑块状银屑病的疗效及安全性
2021-10-11 MedSci原创 MedSci原创
Bimekizumab是一种单克隆IgG1抗体,可选择性地抑制白细胞介素-17A和白细胞介素-17F。在中度至重度斑块状银屑病患者中,bimekizumab与secukinumab相比,其疗效和安全性
Bimekizumab是一种单克隆IgG1抗体,可选择性地抑制白细胞介素-17A和白细胞介素-17F。在中度至重度斑块状银屑病患者中,bimekizumab与secukinumab相比,其疗效和安全性尚未得到广泛的研究。
在这项3b期试验中,我们以1:1的比例随机分配中重度斑块状银屑病患者,以每4周320毫克的剂量皮下注射bimekizumab,或以每周300毫克的剂量皮下注射secukinumab至第4周,随后每4周一次,至第48周。在第16周,接受bimekizumab的患者按1:2的比例重新随机化,接受每4周或每8周一次的维持剂量,直至第48周。主要终点是在第16周,银屑病面积和严重程度指数(PASI)得分比基线减少100%。主要分析首先是测试bimekizumab与secukinumab的非劣效性,幅度为-10个百分点,然后测试其优劣性。
结果,共筛选1005名患者,743名患者入选;373名患者接受bimekizumab,370名接受secukinumab。在第16周,bimekizumab组共有230名患者(61.7%),secukinumab组有181名(48.9%),PASI评分(PASI 100)比基线减少100%(校正后的风险差异,12.7个百分点;95%置信区间[CI],5.8至19.6);bimekizumab显示非劣效,优于secukinumab(非劣效性和优效性的P<0.001)。在第48周,共有250名接受bimekizumab治疗的患者(67.0%)有PASI 100的反应,而接受secukinumab治疗的患者为171名(46.2%)(校正后的风险差异,20.9个百分点;95%CI,14.1-27.7;P<0.001)。在第4周的时间点,bimekizumab组的265名患者(71.0%)的PASI评分比基线减少75%或更多,而secukinumab组的175名患者(47.3%)(校正后的风险差异,23.7;95%CI,17.0-30.4;P<0.001)。使用bimekizumab(72名患者,19.3%)比使用secukinumab(11名患者,3.0%)更经常发生口腔念珠菌病。
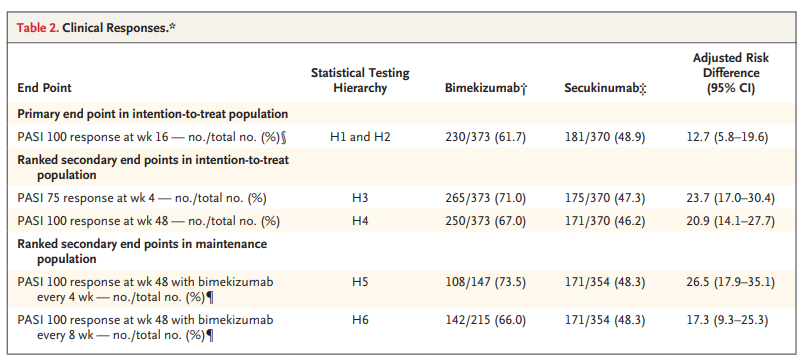
综上所述,该研究结果表明,在中重度银屑病患者中,使用bimekizumab治疗16周和48周后,皮肤清除率高于secukinumab治疗,但与口腔念珠菌病(主要是研究人员记录的轻度或中度)有关。需要更长时间和更大的试验来确定白细胞介素-17抑制剂对银屑病的比较效果和风险。
原始出处:
Kristian Reich, et al., Bimekizumab versus Secukinumab in Plaque Psoriasis. N Engl J Med. 2021 Jul 8;385(2):142-152. doi: 10.1056/NEJMoa2102383.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#MEK#
51
#mAb#
56
#斑块#
49
#斑块状银屑病#
47
#Secukinumab#
42