Cell Death Differ:GLI1通过mTOR/S6K1信号级联反应介导软骨肉瘤的发生发展
2021-03-01 xiaozeng MedSci原创
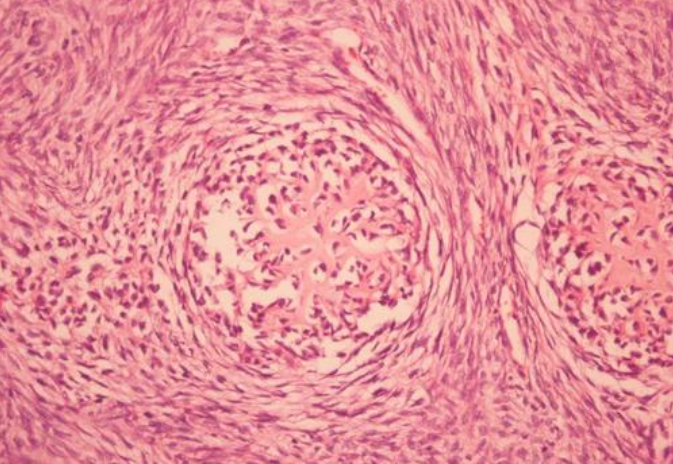
软骨肉瘤(CS)是原发性软骨恶性肿瘤的一种异质性类型,其特征在于肿瘤性软骨形成细胞的积累。
软骨肉瘤(CS)是原发性软骨恶性肿瘤的一种异质性类型,其特征在于肿瘤性软骨形成细胞的积累。约85%的CS病例属于原发性病例。目前,手术切除仍是该恶性肿瘤的一种标准的干预措施。
然而,由于化疗和放疗的作用有限,使得患者的预后仍具挑战。因此,迫切需要鉴定新的治疗靶标并开发有效的联合治疗策略。
既往研究显示,Hedgehog(HH)信号在胚胎发育和产后生物学过程等各个方面均起着至关重要的作用。且该通路的异常以及下游转录因子GLI1的过度表达与包括CS在内的多种恶性肿瘤高度相关。先前的研究显示,敲低GLI1的表达能够抑制CS细胞的存活。然而,调节GLI1表达的潜在机制尚不清楚。
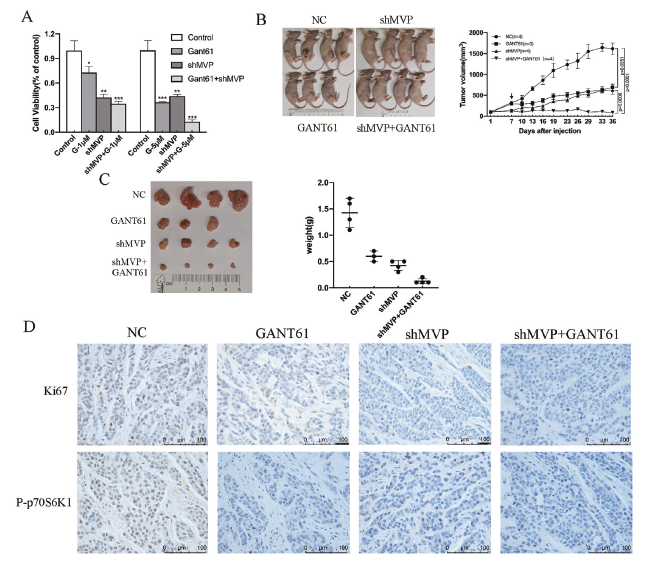
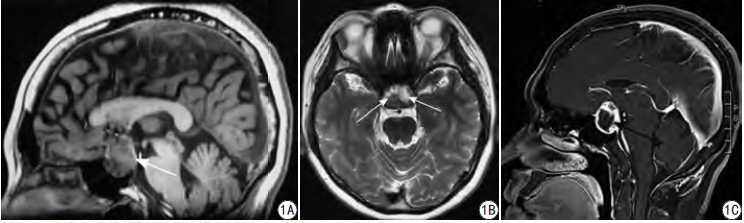
同时抑制MVP和GLI1显著抑制CS的生长
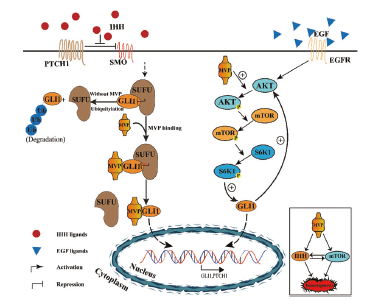
在该研究中,研究人员证实了在CS细胞中GLI1参与了SMO非依赖性信号通路的意义。通过亲和纯化实验,研究人员鉴定了MVP蛋白为GLI1的结合蛋白。MVP能够通过抑制GLI1与SUFU抑制剂的亲和力来促进GLI1的核转运和稳定,并通过mTOR/S6K1信号级联反应来增加GLI1的表达。
相关示意图
功能研究显示,敲低MVP的表达能够抑制细胞的生长并诱导细胞凋亡作用。同时抑制MVP和GLI1会显著抑制CS的生长。此外,进一步的研究显示,MVP、GLI1和P-p70S6K1在71个人源CS组织中高表达。
总而言之,该研究结果揭示了一种独立于HH信号通路的影响GLI1表达的新型调节机制,并为晚期CS患者的联合治疗提供了一定的理论依据。
原始出处:
Wang, W., Yan, T., Guo, W. et al. Constitutive GLI1 expression in chondrosarcoma is regulated by major vault protein via mTOR/S6K1 signaling cascade. Cell Death Differ (26 February 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cell#
26
#Differ#
40
#CEL#
0
#发生发展#
32
太玄乎了,
70
#Death#
48
这是官方的文章吗
83