JACC:Takotsubo综合征的远期预后研究
2018-08-17 MedSci MedSci原创
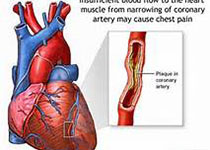
目前,由于临床资料的局限性,关于Takotsubo综合征(TTS)的远期预后尚不清楚。本研究的目的旨在比较和评估TTS和急性冠脉综合征(ACS)患者的预后,并基于不同的触发因素评估TTS的短期和长期预后情况。本研究纳入了1613名TTS患者,并将其与年龄和性别相匹配的ACS患者进行预后情况的比较。在1613名TTS患者中,有485名(30%)患者的触发因素为情感因素,630名(39%)患者的触发因
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#远期预后#
31
#JACC#
0
#ACC#
25
#综合征#
35
#Takotsubo#
30
学习了,涨知识!
56