Arch Gynecol Obstet:多囊卵巢综合症青少年和成年女性之间代谢和肥胖生物标志物的差异
2021-04-16 MedSci原创 MedSci原创
对患有多囊卵巢综合症(PCOS)的妇女的青少年和成年表型的了解可能会推动适时的管理。近日,一项观察性研究比较了青春期和成年PCOS女性的代谢和肥胖生物标志物,研究结果已发表于Arch Gynecol
对患有多囊卵巢综合症(PCOS)的妇女的青少年和成年表型的了解可能会推动适时的管理。近日,一项观察性研究比较了青春期和成年PCOS女性的代谢和肥胖生物标志物,研究结果已发表于Arch Gynecol Obstet。

研究纳入了患有PCOS的62名青少年和 248名成年女性,比较了肥胖和代谢紊乱的生物标志物。使用单变量和多变量二元逻辑回归分析研究了代谢综合征(MS)的预测因素。
青少年和成年PCOS患者平均年龄分别为16.8±1.6岁和28.2±4.8岁(P<0.001)。青少年的月经年龄为11.9±1.3岁,因此该组月经后平均年龄为4.9±0.03岁。青少年的收缩压(112.3 mmHg vs 117.0 mmHg,p = 0.001)和舒张压(70.7 mmHg vs 75.8 mmHg,p <0.001)低于成人。两组中葡萄糖不耐受(12.0% vs 19.3%)和胰岛素抵抗(18.2% vs 17.7%)相似(p > 0.05)。青少年组空腹血糖受损的比例较低(1.8% vs 11.6%,p = 0.015)。青少年的总胆固醇和低密度脂蛋白胆固醇也较低(p<0.001)。青少年和成人的MS分别为10.3%和27.8%(p = 0.005)。内脏脂肪指数(VAI)是青少年(OR = 12.2)和成人(OR = 9.7)MS的良好预测因素。
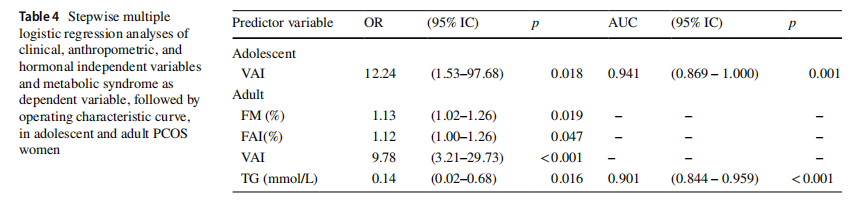
综上所述,该研究结果表明,大多数糖代谢异常的生物标志物在青少年和成人PCOS中相似。青少年的MS患病率较低。在患有PCOS的青少年和成年妇女中,VAI是代谢综合征的有力预测因子。
原始出处:
Sebastião Freitas de Medeiros, et al., Comparison of metabolic and obesity biomarkers between adolescent and adult women with polycystic ovary syndrome. Arch Gynecol Obstet. 2021 Mar;303(3):739-749. doi: 10.1007/s00404-020-05867-x.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#TET#
48
#标志物#
42
#NEC#
36
#多囊卵巢#
40
#多囊卵巢综合症#
39
#生物标志#
27
#生物标志#
27
好文章!
50