基层常见的室性早搏,如何评估和规范化管理?
2022-07-04 MedSci原创 MedSci原创
新版《共识》再次推荐参松养心胶囊用于室早的治疗。《共识》指出:参松养心胶囊经国内多个随机、双盲对照的多中心临床试验证实,其可有效减少室早数量,改善室早患者相关临床症状。
室性早搏简称室早,是临床上最为常见的室性心律失常之一。流行病学资料显示,室早在普通人群中的发病率为1%~4%;体表心电图筛查发现室早患病率约为1%,24h或48h动态心电图检测可高达40%~75%。室早一方面有可能会诱发恶性心律失常,导致心脏的骤停;另一方面对于心功能不全的患者,如果频发、多发的室早会加重心脏负担,加速心力衰竭的发生。
基层是心律失常等慢性疾病的主战场。为了让广大基层医生能更好地认识室性早搏,提高诊断与治疗水平,降低室性心律失常死亡率,由中国农村卫生协会主办的“健康中国,赋能县域”—全科医师系列培训课程第二十四期,特邀武汉大学人民医院赵庆彦教授就室性早搏的病因、诊断及治疗等内容进行了细致分享和权威讲解。
室早的病因
赵庆彦教授首先介绍了室早的病因,主要归纳有三种:
1.各种结构性心脏病,如冠心病、心肌病、心脏瓣膜病导致心室扩张或肥厚、先天性心脏病外科修补后,以及各种心衰等,都可导致室性早搏发生;
2.精神紧张、过度劳累、过量烟、酒、咖啡等不良生活习惯也会诱发室早;
3.药物导致室性早搏的原因:洋地黄类药物、奎尼丁、三环类抗抑郁药物中毒,电解质紊乱(低钾、低镁)等也可导致室早的发生。
表现差异大,室早应科学诊断早干预
“室早的临床表现个体差异很大”,赵庆彦教授指出,临床上许多患者并无明显症状,而有的患者会有心悸、胸闷、心跳停搏感,部分患者有乏力、气促、头晕、黑矇的症状,甚至会诱发心绞痛发作。所以需要依据标准的诊断流程来确定患者是否发生室早。
室早的诊断主要依靠心电图和动态心电图,标准12导联心电图上的室早形态有助于判断室早的起源部位,动态心电图可记录一定时间段的室早总数、昼夜不同时间段的分布情况及其与运动的关系。除此之外,运动试验有助于一些室早患者的病因诊断,若在运动试验中出现多形性室速,则考虑儿茶酚胺敏感性多形性室速的诊断。
室性早搏心肌病在早期很难识别,室性早搏有效消除后心功能和结构得到逆转,则考虑诊断为室性早搏心肌病。即频发室早(24h室早负荷超过总心搏数的15%)可导致心脏扩大、心功能下降,室早根除后心功能可改善(LVEF提高10%)、心脏扩大可逆转,排除其他原因或其他类型心肌病后,可诊断为室早心肌病。
室早都需要治疗吗?
赵庆彦教授强调,并不是所有的室早都需要治疗,对于低危、室早负荷<10%或室早<10000次/24h的无症状患者,通常无需药物治疗。患者应当消除顾虑,避免饮用浓茶、过量饮酒或咖啡等,改善睡眠,调整心态,逐渐会恢复正常心律。对于有可逆性因素如低钾、感染等,应该及时纠正,解决诱因后室早也会得到改善。
对于需要治疗的室早患者,治疗方式一般分为药物治疗和非药物治疗两种。非药物治疗主要指射频导管消融术,但是对于基层医疗卫生机构来说,无论从经济学、治疗效果还是我国医疗资源配置上,室性心律失常的药物治疗地位仍然不可撼动。
近日,由中华医学会心电生理和起搏分会与中国医师协会心律学专业委员会组织国内专家撰写了《室性心律失常中国专家共识基层版》(以下简称《共识》)正式发布。《共识》旨在让基层医院的医生能更好地认识室性心律失常,提高诊断与治疗水平,降低室性心律失常死亡率,促进我国基层医生规范化诊治室性心律失常。
《共识》指出,对于无结构性心脏病室早患者,可选用β受体阻滞剂、美西律、普罗帕酮、非二氢吡啶类钙通道阻滞剂如维拉帕米(维拉帕米使用期间应注意心率和血压变化)。对于结构性心脏病室早患者,可应用β受体阻滞剂和美西律进行治疗。上述药物无效的室早可选择索他洛尔,应用时注意心率、血压和QT间期。需要强调的是,普罗帕酮不能用于合并有冠心病的室早患者,胺碘酮长期应用副作用明显,一般也不推荐用于室早患者。
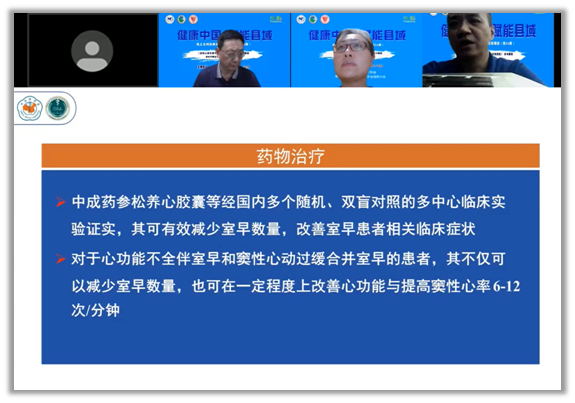
赵庆彦教授介绍,新版《共识》再次推荐参松养心胶囊用于室早的治疗。《共识》指出:参松养心胶囊经国内多个随机、双盲对照的多中心临床试验证实,其可有效减少室早数量,改善室早患者相关临床症状。对于心功能不全伴室早和窦性心动过缓合并室早的患者,其不仅可以减少室早数量,也可在一定程度上改善心功能与提高窦性心律6-12次/分钟。
参松养心治疗室性早搏多中心、随机、双盲临床研究(SS-CAT)证实,参松养心胶囊对于非器质性室早和器质性室早均有效,且可明显减低室早次数并改善心功能。因此《2020室性心律失常中国专家共识》推荐:对于合并或未合并结构性心脏病的症状性室早患者,可考虑使用参松养心胶囊治疗(Ⅱa,A)。对于充血性心力衰竭患者,可考虑应用参松养心胶囊以降低室早负荷,改善心功能。
“健康中国,赋能县域”项目作为行业内提升基层卫生人员和县域及城市社区全科医生诊疗水平的全国性公益项目,致力于对医务专业人员不断加强继续教育,全面提升基层慢病诊疗水平。迄今为止,“健康中国,赋能县域”项目已在线上线下召开11879场,覆盖人群达480521人次,惠及15省的县级医疗卫生机构,真正发挥了引领基层医疗机构慢病管理的作用,该项目将持续发力,助推基层医疗发展,获益广大基层居民。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#规范化#
31
#规范化管理#
43
#室性早搏#
39
#早搏#
45