Liver Cancer:帕博利珠单抗(Pembrolizumab)二线应用于晚期肝癌疗效:来自KEYNOTE-240亚洲人群的亚组分析结果
2021-05-10 yd2015 MedSci原创
亚洲人群晚期肝癌患者二线应用帕博利珠单抗有效并且毒性可耐受
KEYNOTE-240 是一项双盲、安慰剂对照、随机的3期研究。主要评估帕博利珠单抗对比安慰剂二线治疗索拉菲尼失败晚期肝癌的有效性和安全性。患者随机2:1进入帕博利珠单抗(200mg/次/3周)和对照组,直至进展,不能耐受毒性或自动退出研究,或接受35周期(2年)治疗。主要研究终点为无进展生存(PFS)和总生存(OS);次要终点为疾病进展时间(TTP)、客观缓解率(ORR)、疾病控制率(DCR)和反应持续时间(DOR)。
本研究主要分析亚洲人群帕博利珠单抗的有效性以及安全性。一共纳入了157例患者,其中帕博利珠单抗组为107例,对照组为50例。两组基线以及临床特征基本相似。截止2019年1月2日,中位随访时间帕博利珠单抗组为13.8个月,对照组为8.3个月。
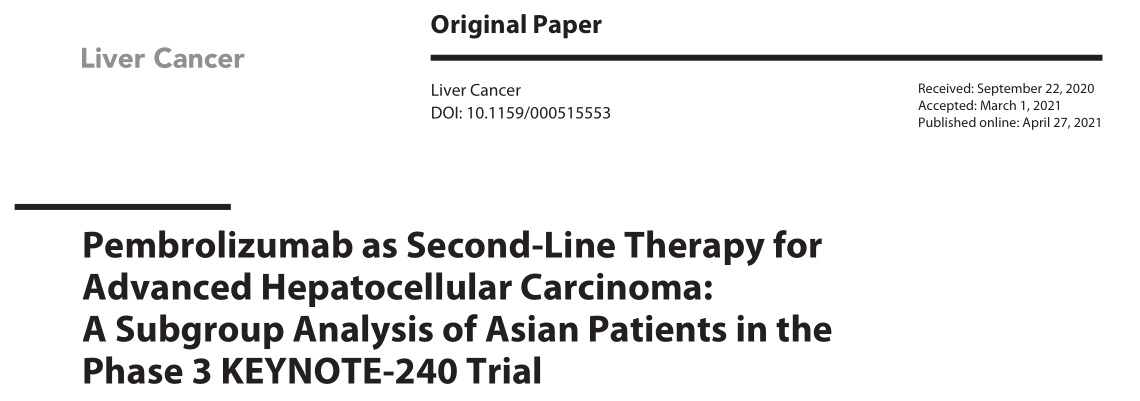
中位PFS:帕博利珠单抗组对比对照组为2.8个月vs 1.4个月(HR=0.48,95% CI 0.32–0.70,p<0.0001)。
PFS
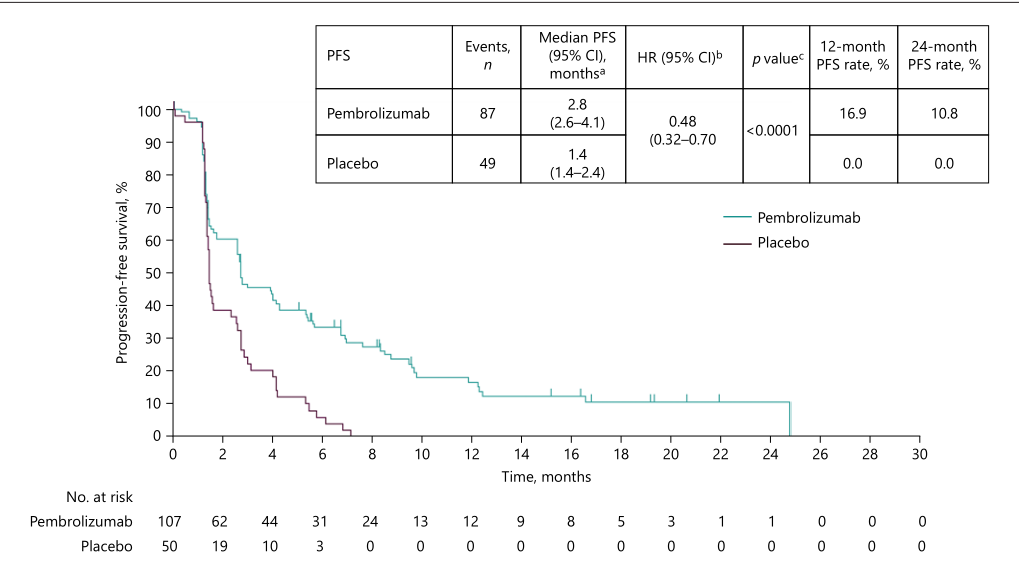
中位OS:帕博利珠单抗组对比对照组为13.8个月vs 8.3个月(HR 0.55; 95% CI 0.37–0.80, p<0.0009)。
OS
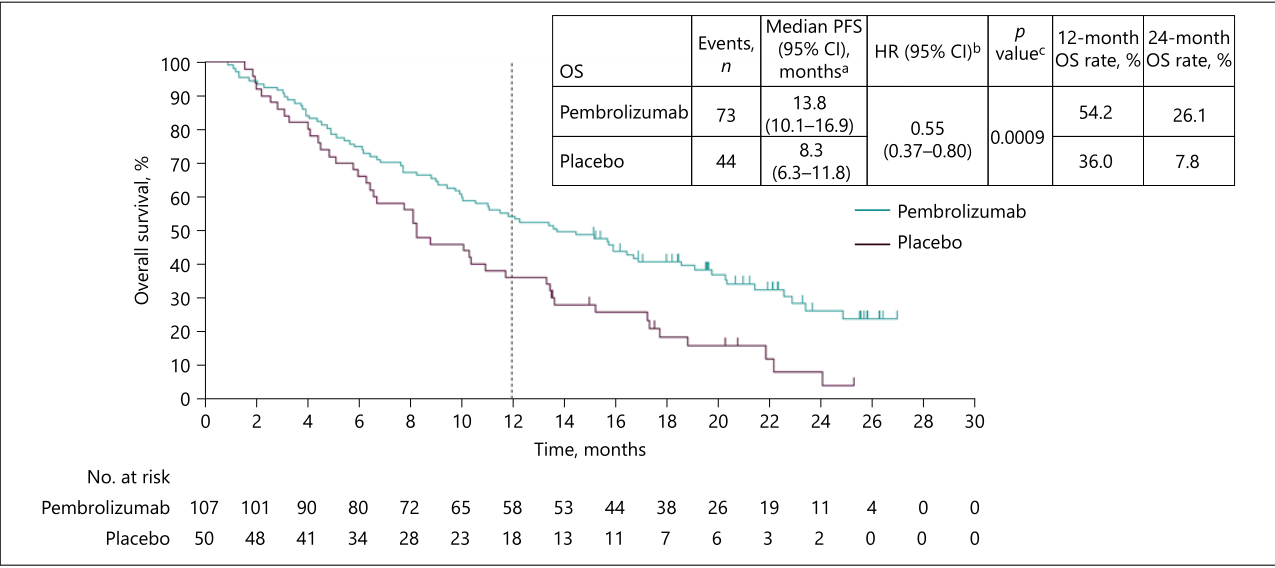
ORR:帕博利珠单抗组对比对照组为20.6% vs 2.0%(相差: 18.5%; 95% CI 8.3–27.6,p=0.0014);DOR:帕博利珠单抗组对比对照组为8.6个月 vs 2.8个月。DCR:帕博利珠单抗组对比对照组为59.8% vs 40.0%(相差: 20.1%; 95% CI 3.1–35.7,p=0.0101)。
临床获益率
任何级别治疗相关不良事件:帕博利珠单抗组对比对照组为58.9% vs 48.0%。3-5级治疗相关不良事件:帕博利珠单抗组对比对照组为13.1% vs 4.0%。无治疗相关死亡病例发生。

治疗相关不良事件
综上,帕博利珠单抗二线治疗晚期肝癌亚洲人群有效并且毒性可耐受。
原始出处:
Masatoshi Kudo, Ho Yeong Lim, Ann-Lii Cheng, et al. Pembrolizumab as Second-Line Therapy for Advanced Hepatocellular Carcinoma:A Subgroup Analysis of Asian Patients in the Phase 3 KEYNOTE-240 Trial. Liver Cancer. 2021. https://doi.org/10.1159/000515553。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#PE#
40
#KEYNOTE#
59
#帕博利珠#
44
#mAb#
49
#Pembro#
42
#Pembrolizumab#
37
#亚洲人群#
40
谢谢梅斯提供这么好的信息,学到很多
64
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
60