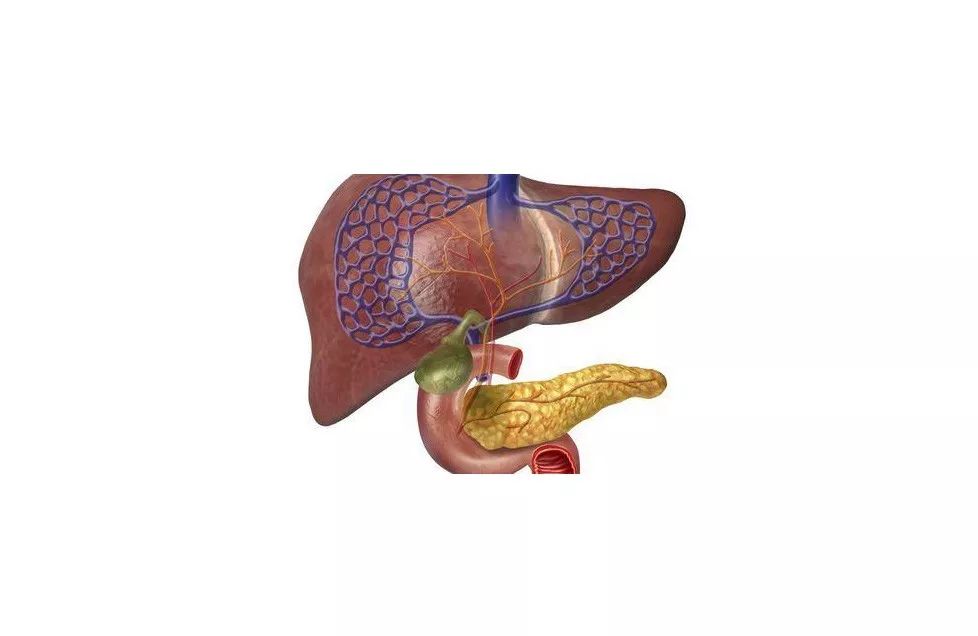
使用活体显微镜观察活体样品中的真菌感染进程而享誉世界的专家,马里兰大学兽医系副教授史美清继续在该领域取得新突破。近日,史美清教授及其团队发表在《Nature Communications》的研究表明,一种叫做Kupffer细胞(KC)的肝巨噬细胞会捕获血液中潜在的致命真菌,然后再传播到诸如大脑或肾脏等的目标器官。该机制不仅解释了为什么肝病患者感染真菌的几率更大,也为今后预防真菌感染和侵袭性真菌感染提供了治疗选择,通过这些选择可以使全球每年150万的人免于死亡。
真菌感染每年影响全球12亿人。在这篇论文中,史美清专门研究了两种真菌——新型隐球菌和白色念珠菌。这两种真菌,如果传播到它们的目标器官(隐球菌-大脑和念珠菌-肾脏),一旦感染就很难治疗。例如,隐球菌是脑膜炎的主要病因。每年有100多万人感染脑膜炎,其中有60%将死于该病。
“隐球菌和念珠菌实际上是无处不在的真菌,”史美清说。“拥有健康免疫系统的人通常可以在感染后控制真菌,但一旦进入血液,这些真菌中的任何一种都可以进入目标器官并致命。对于免疫系统受损的患者,如HIV患者或器官移植患者,隐球菌尤其是个问题。肝病患者也更容易感染隐球菌,但之前没有人知道为什么。”
KCs或肝巨噬细胞负责捕捉血液中游离的真菌防止进一步传播有助于解释这一现象,因为如果肝病患者肝脏受损了,这样解释也合乎道理,这种保护机制也会受损。
“这个发现很有趣,也很不寻常,因为在真菌感染领域,没有人关注肝脏,”史美清说。研究人员倾向于研究目标器官,如大脑或肾脏。肝脏不是目标器官,但它试图清除血液中的真菌。由于人体是相互联系的,因此本文对真菌在人体中如何相互作用提供了一个更完整的系统方法。
考虑到这种全身的方法,这种机制的发现不仅对肝病患者有意义,而且可以通过靶向这种机制,防止真菌传播和治疗侵袭性真菌感染治疗整体真菌感染。
原始出处:
Donglei Sun, Peng Sun, Hongmei Li, et al. Fungal dissemination is limited by liver macrophage filtration of the blood. Nature Communications volume 10, Article number: 4566 (2019).
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
0
#COMMUN#
29
#真菌#
36
#真菌感染#
43
#侵袭性#
24
#研究团队#
38