Cancer Cell:吴一龙,周清教授发现靶向联合抗血管新生对EGFR突变NSCLC患者获益显著(ARTEMIS-CTONG1509研究)
2021-08-14 MedSci原创 MedSci原创
肺癌是中国发病率和死亡率最高的恶性肿瘤,多数患者在诊断时已是晚期疾病,严重威胁生命健康。8月12日,由广东省人民医院终身主任、广东省肺癌研究所名誉所长吴一龙教授牵头,周清教授作为研究的主要承担者,对携
肺癌是中国发病率和死亡率最高的恶性肿瘤,多数患者在诊断时已是晚期疾病,严重威胁生命健康。8月12日,由广东省人民医院终身主任、广东省肺癌研究所名誉所长吴一龙教授牵头,周清教授作为研究的主要承担者,对携带EGFR突变的非小细胞肺癌患者中进行的Ⅲ期研究——ARTEMIS—CTONG 1509的研究结果在国际知名学术期刊《细胞·癌症》(Cancer Cell)上在线发表。
这项研究证实,对于携带EGFR突变且未经治疗的非小细胞肺癌晚期患者,采用贝伐珠单抗联合厄洛替尼的治疗方法,相比传统的厄洛替尼单药治疗,可以显著延长患者的无进展生存期,对于21外显子L858R点突变患者和脑转移患者,采用这一疗法的获益更为明显。
联合治疗将此类患者的中位无进展生存期由11.2个月延长至17.9个月,疾病进展风险降低了45%,且该疗法的毒性可管理、可耐受,可作为晚期、转移性或复发的EGFR突变阳性非小细胞肺癌患者的一线治疗选择。

探索厄洛替尼与其他药物的联合治疗策略
肺癌分为非小细胞肺癌和小细胞肺癌,其中非小细胞肺癌约占所有肺癌的80%。在非小细胞肺癌中,有30%-40%的患者会携带表皮生长因子受体(EGFR)基因突变。

虽然靶向治疗,如厄洛替尼可以使这类患者受益,但是大部分接受厄洛替尼单药治疗的患者会出现耐药性,导致治疗失败。同时,不同临床特征、不同突变亚型的患者在单药治疗中的获益程度不同。最为典型的是,出现脑转移比没有出现脑转移的患者在厄洛替尼单药治疗中的获益少。常见的两种突变亚型中,19外显子缺失突变亚型与21外显子L858R点突变相比,21外显子L858R点突变的患者用单药治疗的疗效更差。
如何提高疗效,尤其是在厄洛替尼单药中获益相对较小的特殊人群的疗效?吴一龙团队开始探索厄洛替尼与其他药物的联合治疗策略。ARTEMIS-CTONG1509应运而生。
2015年,ARTEMIS-CTONG1509研究启动,在全国14个中心选取311例携带EGFR突变、未经治疗的非小细胞肺癌晚期患者,分别进行贝伐珠单抗联合厄洛替尼与厄洛替尼单药治疗,研究对比两种疗法的疗效和安全性。
2019年的欧洲肿瘤内科学会年会(ESMO)上,广东省肺癌研究所副所长周清教授代表研究团队发布了ARTEMIS-CTONG1509研究的临床数据特色以及转化性研究成果。
研究结果显示,贝伐珠单抗联合厄洛替尼治疗能显著延长患者无进展生存期,中位无进展生存期达17.9个月,比厄洛替尼单药治疗(11.2个月)延长超过半年,患者的疾病进展风险降低了45%。
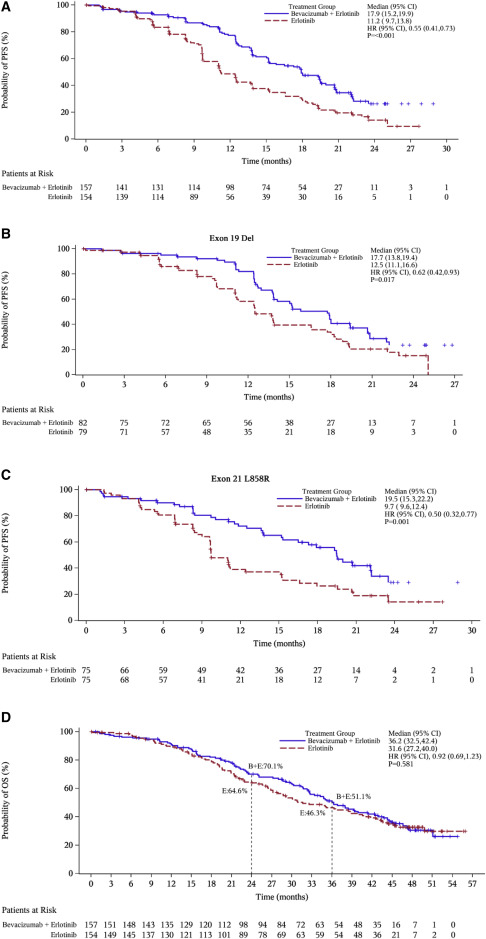
与此同时,研究发现携带21外显子L858R点突变的患者在联合治疗中的获益不仅大于厄洛替尼单药治疗,其获益程度也超过了19外显子缺失突变患者从联合治疗中的获益。在脑转移的患者中,联合治疗不仅显著延长了无进展生存期,甚至具有延长总生存期的趋势,入组患者3年的总生存率从30.6%提高到43%。

由此可见,联合治疗对于21外显子L858R点突变的患者和脑转移患者具有更好的疗效。
在不良反应的观察中,研究团队发现,联合治疗组中两种药物的不良反应叠加。周清表示,贝伐珠单抗常见的不良反应是高血压和蛋白尿,两种不良反应在治疗中的程度是基本可控的,临床医生此也具备多年的处理经验,对病人的生活质量影响是比较小。总体而言,贝伐珠单抗联合厄洛替尼治疗的毒性可管理且可耐受,研究中也尚未观察到新的安全性事件。
日本同期进行的一项几乎同样内容的研究也证实联合治疗的有效性。与日本的研究相比,ARTEMIS-CTONG1509研究增加分析了联合治疗对21外显子L858R点突变和脑转移患者的疗效和安全性,在特殊人群的研究上具有独创性。
去年,贝伐珠单抗联合厄洛替尼治疗已被写入中国临床肿瘤学会《原发性肺癌诊疗指南》(2020年版),成为EGFR基因突变患者的一线治疗选择之一。
吴一龙表示,目前贝伐珠单抗、厄洛替尼两种靶向治疗药物均已纳入广州市医保范围,患者报销后每个月需要的治疗费用大约2000多元。这一治疗方案广泛应用后将惠及更多患者。
对于肺癌的救治,吴一龙和团队还有很多新想法等待验证,包括探索各种联合治疗的方法,从耐药机制入手预防耐药出现,探讨间歇性治疗的可能性,还有寻找新的治疗策略。“最近有一些研究正在准备启动。如果这四个方面在未来十年可以实现一个,都将是非常了不起的成就。”吴一龙说。
原始出处:
Qing Zhou, Chong-Rui Xu, Ying Cheng, Yun-Peng Liu, Gong-Yan Chen, Jiu-Wei Cui, Nong Yang, Yong Song, Xiao-Ling Li, Shun Lu, Jian-Ying Zhou, Zhi-Yong Ma, Shi-Ying Yu, Cheng Huang, Yong-Qian Shu, Zhen Wang, Jin-Ji Yang, Hai-Yan Tu, Wen-Zhao Zhong, Yi-Long Wu. Bevacizumab plus erlotinib in Chinese patients with untreated, EGFR-mutated, advanced NSCLC (ARTEMIS-CTONG1509): A multicenter phase 3 study.Cancer Cell, 2021,https://doi.org/10.1016/j.ccell.2021.07.005.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#抗血管#
56
#CTO#
49
#cancer cell#
56
#Cell#
36
#血管新生#
49
#ARTEMIS#
42
#SCLC患者#
29
#CEL#
37
#ART#
37
#NSCLC患者#
42