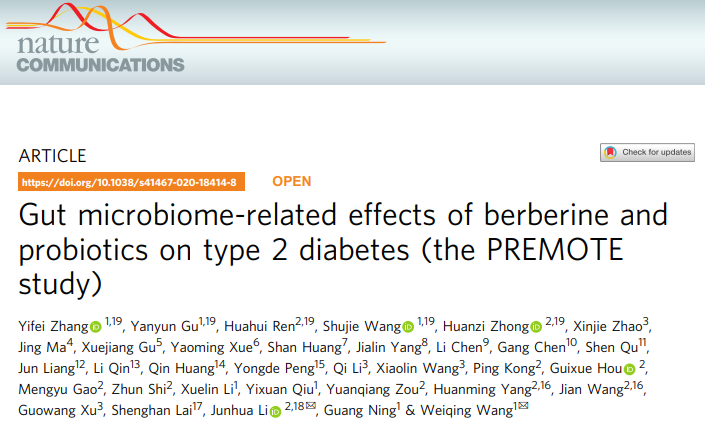
Nat Commun:小檗碱和益生菌对2型糖尿病肠道微生物的影响——PREMOTE研究
2021-07-31 MedSci原创 MedSci原创
肠道微生物组有望用于治疗2型糖尿病(T2D),改变肠道微生物群的措施,如口服益生菌或小檗碱(BBR)有利于代谢的平衡。近日,因此,一项随机、双盲、安慰剂对照试验评估了BBR治疗T2D的效果,研究结果已
肠道微生物组有望用于治疗2型糖尿病(T2D),改变肠道微生物群的措施,如口服益生菌或小檗碱(BBR)有利于代谢的平衡。近日,因此,一项随机、双盲、安慰剂对照试验评估了BBR治疗T2D的效果,研究结果已发表于Nat Commun。
研究纳入来自中国20个中心的新诊断的49名T2D患者,随机分配(1:1:1:1),经过一周的庆大霉素预处理后,完成了为期12周的BBR-单药、益生菌+BBR、益生菌-单药或安慰剂的治疗。
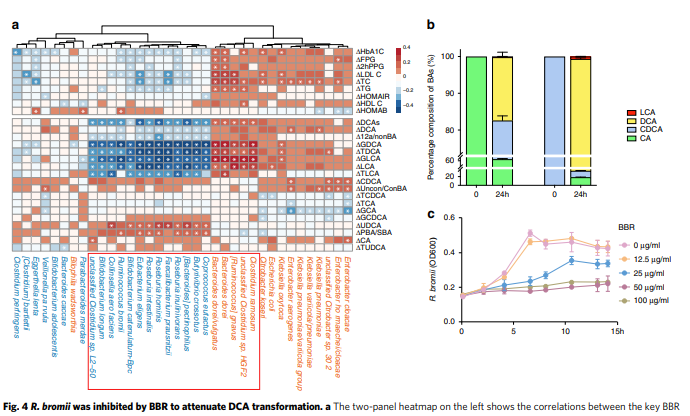
结果显示,作为主要结果,益生菌+BBR(最小二乘法平均值[95% CI],-1.04[-1.19, -0.89]%)和BBR-单药组(-0.99[-1.16, -0.83]%)的糖化血红蛋白变化明显大于安慰剂和益生菌单药组(-0.59[-0.75, -0.44]%, -0.53[-0.68, -0.37]%, P<0.001)。BBR治疗诱发了更多的胃肠道副作用。进一步的元基因组学和代谢组学研究发现,BBR的降血糖作用是由溴化小鼠球菌对DCA生物转化的抑制所介导的。
综上,该研究结果揭示了BBR对T2D的抗糖尿病作用与人类微生物有关。
原始出处:
Yifei Zhang, et al., Gut microbiome-related effects of berberine and probiotics on type 2 diabetes (the PREMOTE study). Nat Commun. 2020 Oct 6;11(1):5015. doi: 10.1038/s41467-020-18414-8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#COMMUN#
25
#微生物#
31
#REM#
38
#Nat#
29
#remote#
21
谢谢MedSci提供最新的资讯
43