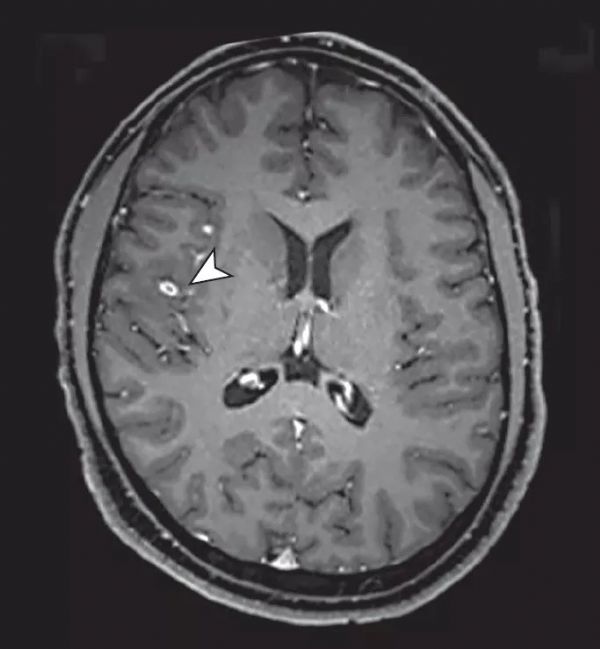
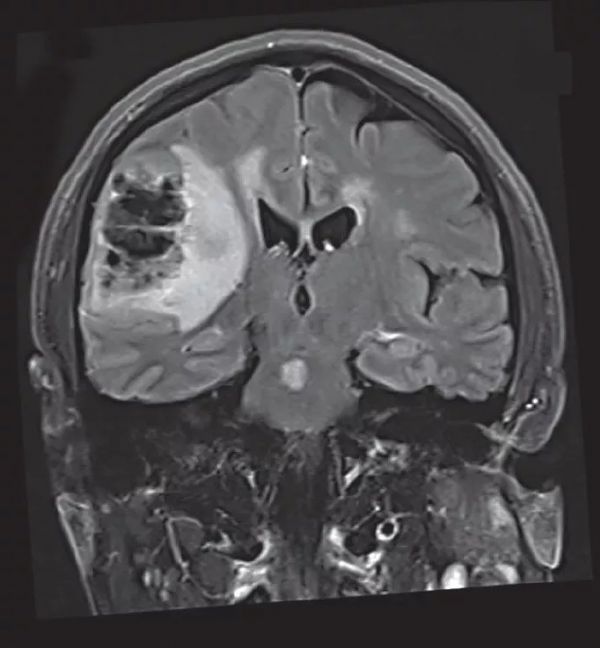
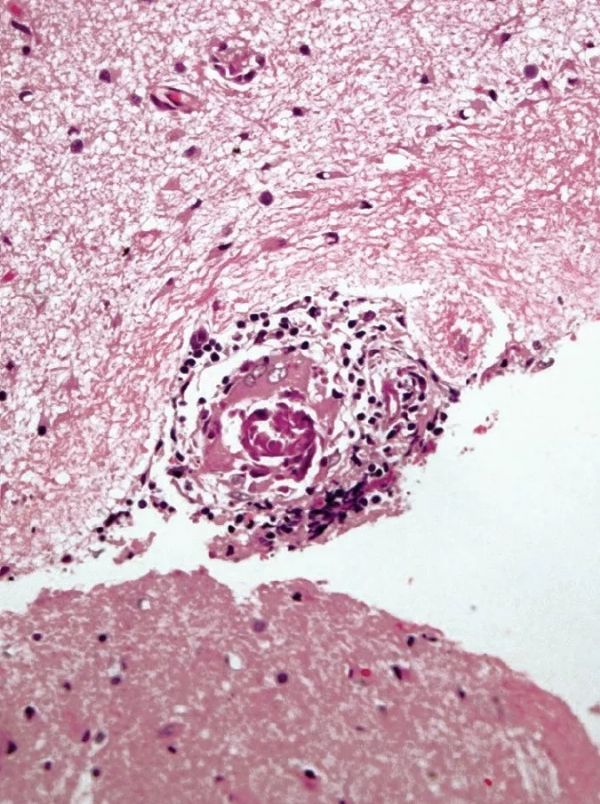
JAMA N:反反复复脑梗死和脑出血什么回事?
2018-06-09 杨中华 脑血管病及重症文献导读
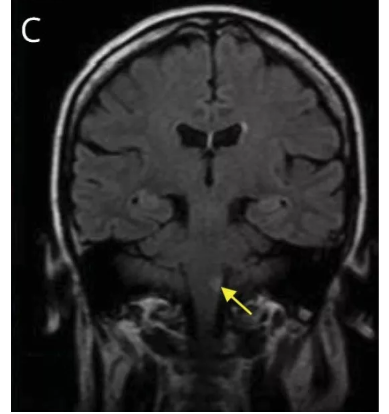
40多岁,男性,印度人。为了评价复发性缺血性卒中和脑出血就诊。 既往病史包括高血压和痛风。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#脑梗#
28
受用了
59
好文献学习了
65
了解一下.谢谢分享!
1
vvv还好还好哈就
57