Brain Behav Immun: 青少年外周炎症与静息状态功能连接的关系
2021-03-08 MedSci原创 MedSci原创
目前关于外周炎症与神经功能关系的研究相对较少。成人神经影像学研究发现外周炎症指标增高与一些情绪、认知相关的静息态功能连接变化有关。很少有研究关注青少年中的这些关联,然而,来自青少年的稀缺数据表明青少年
目前关于外周炎症与神经功能关系的研究相对较少。成人神经影像学研究发现外周炎症指标增高与一些情绪、认知相关的静息态功能连接变化有关。很少有研究关注青少年中的这些关联,然而,来自青少年的稀缺数据表明青少年的网络不同与成人不同。Johnna R. Swartz等在Brain Behav Immun发表文章对青少年外周炎症与静息状态功能连接的关系进行了研究。
目前的研究调查了社区青少年样本(n=70;年龄,12-15岁;女性32人,男性36人)外周炎症与rsFC之间的关系。采血后行fMRI扫描,评估rsFC。检测血清炎症标志物,包括白细胞介素-6(IL-6)、肿瘤坏死因子-α(TNF-α)和C反应蛋白。
研究发现较高的肿瘤坏死因子-α水平与右侧杏仁核与左侧纹状体、右侧额叶下回与左侧顶叶皮质的rsFC改变相关(p<0.0 5),与IL-6和CRP的相关性不显著。
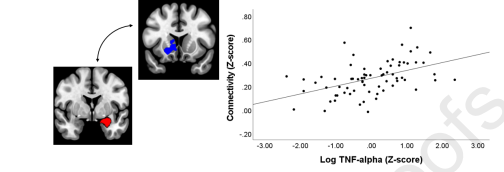
右侧杏仁核功能连接与TNF-α关系
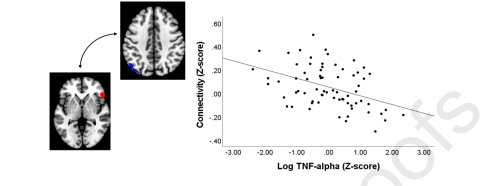
右侧额下回功能连接与TNF-α的关系
与成人的研究结果相比,炎症可能与青春期发育中的大脑的功能连接有独特的联系。研究结果对理解外周炎症如何影响青春期的连通性有一定的意义,因为青春期的神经网络正在经历重大的发育变化。
原文出处:Swartz Johnna R,Carranza Angelica F,Tully Laura M et al. Associations between peripheral inflammation and resting state functional connectivity in adolescents.[J] .Brain Behav Immun, 2021, undefined: undefined.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#静息状态#
34
#HAV#
31
#功能连接#
36
#EHA#
29
学习一下
80
青少年外周炎症
83