Alzheimer's & Dementia:COVID-19住院患者的神经并发症可能与神经退行性生物标志物升高有关
2022-01-23 影像小生 MedSci原创
AD痴呆患者的神经退行性生物标志物水平升高,与住院的COVID-19患者的脑病和更糟的预后相关。
Jennifer A. Frontera等在Alzheimer's & Dementia杂志发表文章,假设在有临床证据表明新发认知功能障碍(特别是毒性代谢性脑病[TME])的住院COVID-19患者中,神经和神经胶质损伤的血液生物标志物将会升高,神经退行性生物标志物的升高与住院死亡风险的升高和出院率的降低有关。进一步的目的是比较住院的COVID患者和具有不同程度认知障碍(正常、轻度认知障碍[MCI]或阿尔茨海默病[AD])的非COVID对照组的神经退行性生物标志物水平,以评估他们的脑损伤程度。
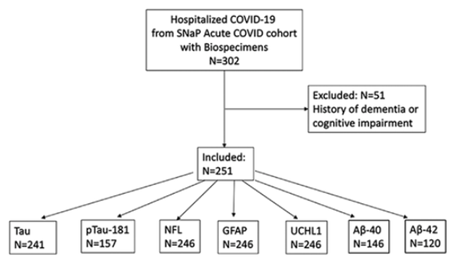
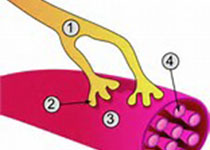
被试纳入过程
对251例无痴呆病史的住院新冠肺炎患者,该研究分析了有或没有脑病的患者,住院死亡与存活,出院回家与其他处置的血清总tau (t-tau)、磷酸化tau-181 (p-tau181)、胶质纤维酸性蛋白(GFAP)、神经丝轻链(NfL)、泛素羧基末端水合酶L1 (UCHL1)、和淀粉样蛋白β (a β40,42)之间的差异。研究人员还将COVID-19患者的生物标志物水平与非COVID-19患者的认知正常、轻度认知障碍(MCI)和阿尔茨海默病(AD)痴呆对照组(N = 161)进行了比较。
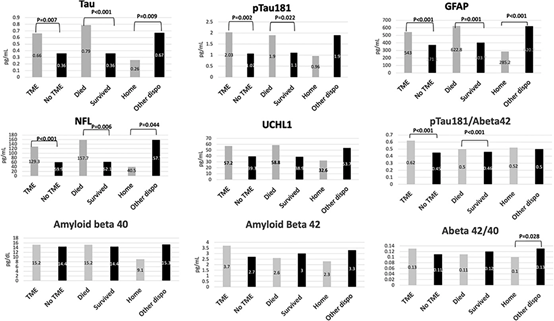
有或无中毒性代谢性脑病(TME)住院的COVID-19患者(N = 251)的血清神经退行性生物标志物、住院死亡与生存、出院回家与其他出院处理的对比。
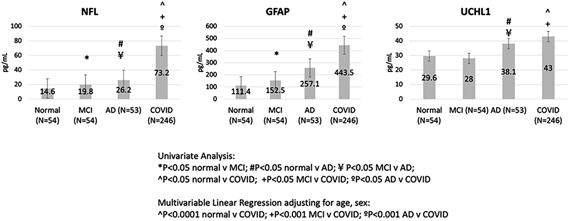
对照组(161例无认知障碍、轻度认知障碍和AD痴呆患者)和住院的COVID患者(251例)的血清生物标志物水平
脑病患者和住院死亡患者入院时t-tau、p-tau181、GFAP和NfL显著升高,出院患者入院时t-tau、GFAP和NfL显著降低。这些标志物与COVID疾病的严重程度相关。
COVID患者的NfL、GFAP和UCHL1高于MCI或AD的非COVID对照组。
血清神经元、胶质和轴突神经退行性生物标志物,包括t-tau、p-tau181、UCHL1、GFAP和NfL,在因COVID-19住院后的脑病患者中显著升高,出院处置更差。这些标志物与COVID疾病的严重程度相关。此外,住院的COVID患者中NfL、GFAP和UCHL1水平与非COVID - 19 AD痴呆患者中观察到的水平相似或更高。有必要进行更多的研究,跟踪这些生物标志物的轨迹,以及它们与COVID-19幸存者的长期认知结果之间的关系。
AD痴呆患者的神经退行性生物标志物水平升高,与住院的COVID-19患者的脑病和更糟的预后相关。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#标志物#
35
#并发#
29
#dementia#
34
#神经退行#
33
#生物标志#
29
#生物标志#
28