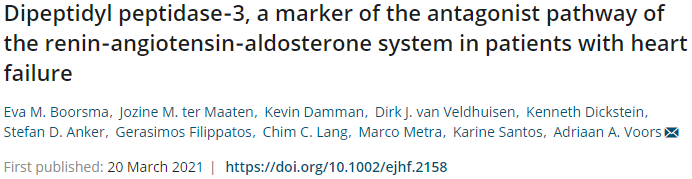
Eur J Heart Fail:二肽基肽酶3,心衰患者RAAS系统拮抗途径的标志物
2021-03-26 MedSci原创 MedSci原创
抗DPP3的特异性抗体Procizumab可能是心力衰竭患者未来潜在的治疗选择
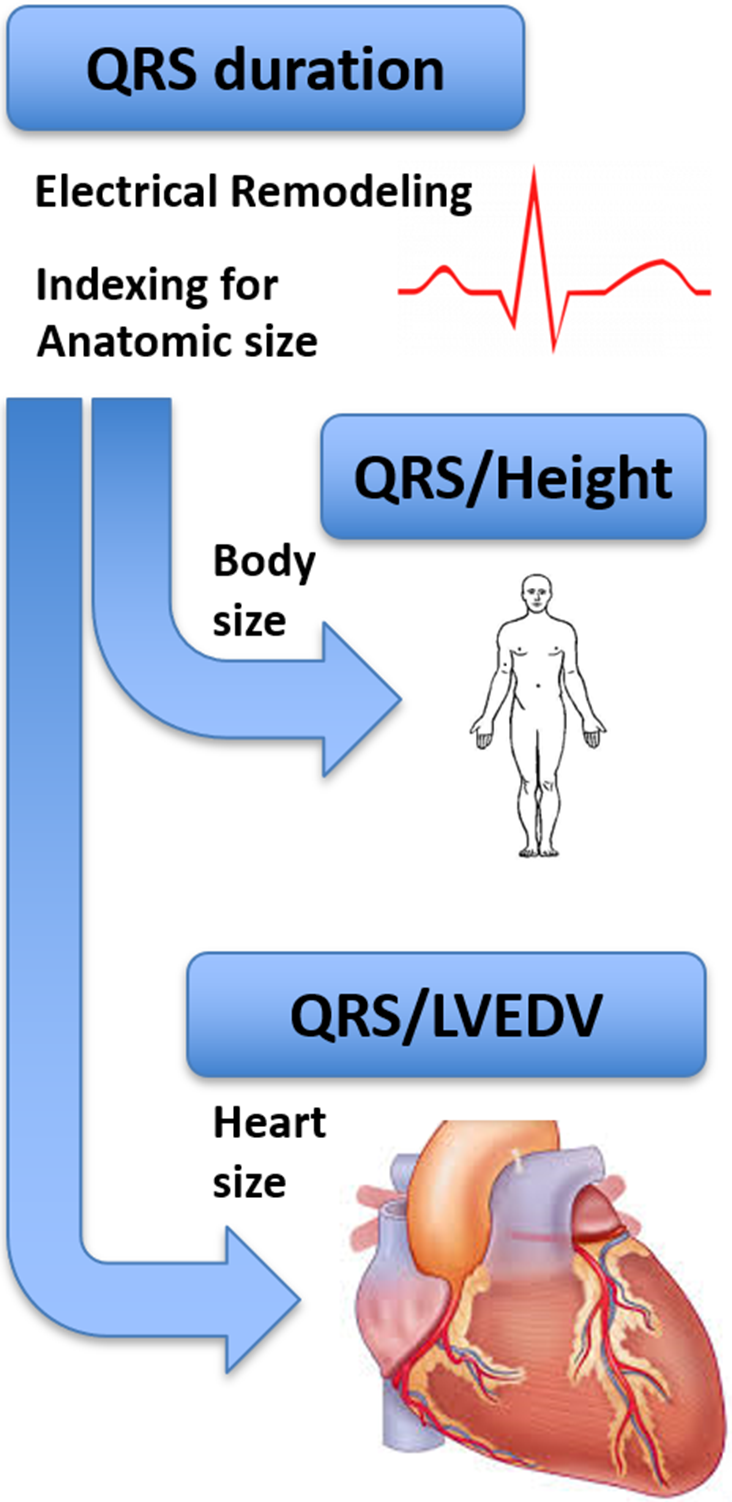
近期研究发现,二肽基肽酶3(DPP3)是负责裂解血管紧张素(1-7)(Ang[1-7])的肽酶。Ang(1-7)是ACEⅡ-血管紧张素(1-7)-Mas(AAM)通路的一部分,被认为可以拮抗肾素-血管紧张素-醛固酮系统(RAAS)。
鉴于DPP3可抑制RAAS的拮抗通路,Boorsma等研究人员推测,DPP3在心力衰竭的发生过程中可能是有害的。但是,目前没有关于慢性心力衰竭患者DPP3的数据。因此,Boorsma等在心力衰竭恶化患者中研究了DPP3浓度升高相关的临床特征和结局。
Boorsma等采用德国亨尼斯多夫4TEEN4制药有限公司生产的DPP3-LIA发光法,对2156例心力衰竭恶化患者的血清标本进行了DPP3测定。
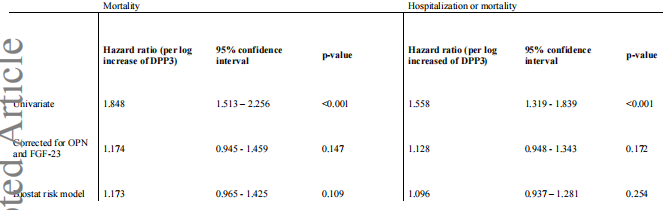
死亡率或联合终点的Cox回归分析
DPP3的中位浓度为11.45 ng/mL,范围为2.8~84.9 ng/mL。DPP3浓度较高的患者具有较高水平的肾素(Q1-3 vs Q4: 78.3 vs 120.7 uI/mL, p<0.001)和醛固酮(88 vs 116 uI/mL,p<0.001)。
对数ALT、对数总胆红素、无糖尿病、骨桥蛋白FGF23和NT proBNP浓度升高都是DPP3浓度升高的最强独立预测因素(所有p<0.001)。在单变量生存分析中,DPP-3与死亡率和死亡或心力衰竭住院的联合终点相关(P<0.001)。但在对混杂因素进行调整后,这种关联的显著性消失。
总结示意图
综上,在心力衰竭恶化的患者中,DPP3是伴随RAAS活性升高的重症疾病的标志物。DPP3或可通过抵消Mas受体通路而使心力衰竭进一步恶化。抗DPP3的特异性抗体Procizumab可能是心力衰竭患者未来潜在的治疗选择。
原始出处:
Boorsma Eva M,Ter Maaten Jozine M,Damman Kevin et al. Dipeptidyl peptidase-3, a marker of the antagonist pathway of the renin-angiotensin-aldosterone system in patients with heart failure. Eur J Heart Fail, 2021, https://doi.org/10.1002/ejhf.2158
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#标志物#
0
学习到了很多东西谢谢老师
79
#RAAS#
51
#ART#
49
#心衰患者#
41
#HEART#
29
好
74