CNStroke2018丨中国心源性卒中的现状与发展——房颤与卒中的新进展
2018-05-08 国际循环编辑部 国际循环
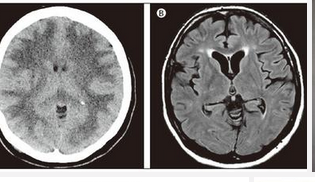
中国脑卒中大会,暨第八届全国心脑血管病论坛2018年5月3~6日在北京召开。现任国家心血管病中心、中国医学科学院阜外医院教授、博士生导师、心律失常诊治中心主任张澍教授,就中国目前心房颤动(房颤)与卒中诊断和治疗的新进展情况发表专题报告。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CNS#
48
#NST#
38
学习了
92
#心源性#
31
谢谢了.学习
97
很好.学习了
91
学习一下谢谢分享
98
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
42
厉害了我的哥
86
谢谢分享学习
23