他汀药物在心血管疾病一级预防中利大于弊
2021-07-17 MedSci原创 MedSci原创
在心血管疾病的一级预防中,他汀类药物引起不良事件的风险较低,且不超过其预防心血管疾病的疗效,表明他汀类药物的利害平衡总体上是有利的。
心血管疾病是世界范围内死亡率和发病率的主要原因。他汀类药物可有效降低心血管疾病的风险,临床指南推荐他汀类药物作为预防心血管疾病的一线治疗。然而,临床使用中报告了各种不良事件,包括肌肉问题、肝功能不全、肾功能不全、糖尿病和眼部疾病。先前的研究表明,他汀类药物的摄取和持续性较差,因此,数以百万计的患者可能会错过挽救生命的治疗。这种使用不足的部分原因是担心潜在的不良反应,当他汀类药物用于无心血管病史的无症状患者的一级预防时,这些担心尤其明显。在这些平均心血管疾病风险较低的个体中,他汀类药物的绝对益处小于既往心血管疾病事件的二级预防人群,因此对治疗平衡的益处可能不太有利,最近的指南建议更广泛地使用他汀类药物进行一级预防,使大量心血管疾病低风险人群有资格接受治疗并暴露于不良反应的风险中。这种增加他汀类药物干预的资格一直存在争议,在一级预防人群中,需要更好地了解不良反应的风险,以确定他汀类药物的益处和危害之间的权衡。
牛津大学纳菲尔德初级保健卫生科学系Ting Cai等探讨他汀类药物与心血管疾病一级预防中不良事件的关系,以及他汀类药物的种类和剂量对不良事件的影响。
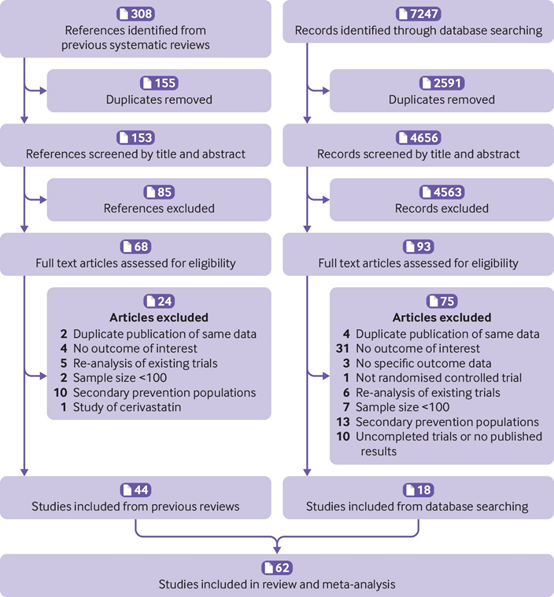
该研究数据来源从以前的综述中确定,并在Medline、Embase和Cochrane中央对照试验登记册中搜索。在无心血管病史的成人中进行的随机对照试验,比较他汀类药物与非他汀类药物对照组,或比较不同类型或剂量的他汀类药物。
主要观察指标为常见不良事件:自我报告的肌肉症状、临床确诊的肌肉疾病、肝功能不全、肾功能不全、糖尿病和眼部状况。次要观察指标包括心肌梗死、中风和心血管疾病死亡作为疗效指标。
该研究进行了成对荟萃分析,计算他汀类药物和非他汀类药物对照组之间的优势比和95%置信区间,以及每10例事件的绝对风险差异 估计一年治疗的病人有1000人。进行网络荟萃分析,比较不同类型他汀类药物的不良反应。基于Emax模型的meta分析被用来检查每种他汀类药物不良反应的剂量-反应关系。
共纳入62个临床试验,其中120456名参与者,平均随访3.9年。他汀类药物与自我报告的肌肉症状风险增加相关(21项试验,优势比1.06(95%可信区间1.01-1.13);绝对风险差15(95%可信区间1~29),肝功能不全21例,比值比1.33(1.12~1.58);绝对风险差8(3:14),肾功能不全(8项试验,比值比1.14(1.01:1.28);绝对风险差12(1-24)),眼部状况(6次试验,优势比1.23(1.04-1.47);绝对风险差异14(2至29),但与临床确诊的肌肉疾病或糖尿病无关。

所有纳入研究的偏倚风险汇总
风险的增加并不超过主要心血管事件风险的降低。阿托伐他汀、洛伐他汀和瑞舒伐他汀单独与一些不良事件相关,但在不同类型的他汀类药物之间没有发现显著差异。阿托伐他汀对肝功能不全的影响存在Emax剂量-反应关系,但其他他汀类药物的剂量-反应关系和不良反应没有定论。
在心血管疾病的一级预防中,他汀类药物引起不良事件的风险较低,且不超过其预防心血管疾病的疗效,表明他汀类药物的利害平衡总体上是有利的。支持在开始治疗前调整他汀类药物的类型或剂量以解决安全问题的证据是有限的。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习
44
#血管疾病#
37
写得好
61
学习学习学习学习学习学习学习
53
学习
46
关注心血管疾病
47
学习
58