Radiology:还是一个年轻人的你,30年后会出现支气管扩张吗?
2021-06-08 shaosai MedSci原创
支气管扩张是一种定义为气道病理性扩大的疾病,在世界范围内被越来越多地认识及关注。支气管扩张的特点是反复循环的炎症和恶化,最终导致气道结构的不可逆损伤。
 支气管扩张是一种定义为气道病理性扩大的疾病,在世界范围内被越来越多地认识及关注。支气管扩张的特点是反复循环的炎症和恶化,最终导致气道结构的不可逆损伤。尽管与支气管扩张风险增加相关的基本因素和条件,例如衰老、感染(例如肺炎,结核病)和囊性纤维化已广为人知,但降低风险的因素仍待探索。
支气管扩张是一种定义为气道病理性扩大的疾病,在世界范围内被越来越多地认识及关注。支气管扩张的特点是反复循环的炎症和恶化,最终导致气道结构的不可逆损伤。尽管与支气管扩张风险增加相关的基本因素和条件,例如衰老、感染(例如肺炎,结核病)和囊性纤维化已广为人知,但降低风险的因素仍待探索。
研究表明,较高水平的心肺功能与延缓肺功能下降及降低气道疾病(如慢性阻塞性肺疾病)发生的风险有关。然而据我们所知,心肺适应性是否能降低支气管扩张的风险尚不明确。
近日,发表在Radiology杂志的一项研究探讨了心肺适应性与支气管扩张之间的关系,为进一步阐明支气管扩张的病理生理及疾病进展提供了参考依据。
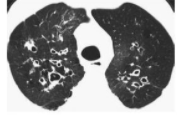
本项前瞻性观察性研究评估了青年队列(1985-1986[0年]至2015-2016[30年])的冠状动脉风险发展。在30年期间,健康参与者(年龄在18-30岁)在第0年和第20年进行了跑步机运动测试。根据跑步机运动时间确定心肺适应性。采用心肺适应性20年的差异作为适应性测量。在第25年,进行胸部CT扫描以评估支气管扩张,并将其作为主要结果。采用多变量logistic模型来确定心肺适应性变化和支气管扩张之间的关系。
在2177名被选参与者(0年:平均年龄25岁±4岁[标准差];1224名女性)中,209名(9.6%)在第25年有支气管扩张。在校正了年龄、种族-性别组、研究地点、体重指数、吸烟年限、结核病、肺炎、哮喘和心肌梗死史、肺功能峰值和心肺适应能力后,在第25年行CT扫描时,心肺适应性的保持与支气管扩张的低风险相关(从第0年到第20年每延长1分钟跑步机时间:优势比[OR],0.88;95% CU: 0.80、0.98;P = .02)。支气管扩张与同时出现咳嗽和痰表现出了较强的相关性(OR, 0.72;95% CI: 0.59, 0.87;P <.001)。
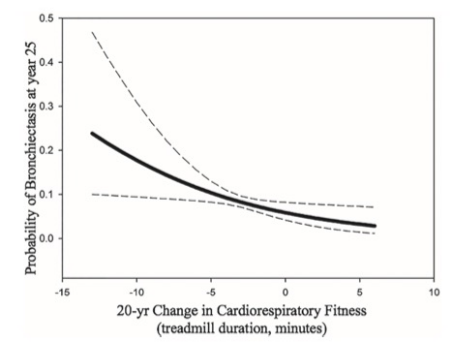
图 该图显示了20年来心肺适应性的变化和第25年CT扫描上支气管扩张的概率。图中显示了多变量分析的拟合线和95%CI(虚线)。第0年到第20年之间的心肺适应性保持与第25年CT时支气管扩张的低概率相关(优势比,0.88;95%CI: 0.80、0.98;P = .02)。
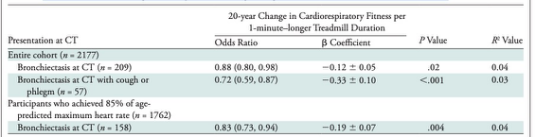
表 20年心肺适应性变化与第25年CT扫描时支气管扩张的相关性。
本研究通过18-30岁健康年轻人的人群队列研究,证实了20年以上心肺适应性保持与第25年CT扫描表现支气管扩张的低发生率相关,当支气管扩张伴有呼吸道症状作为替代结果时,这种相关性更强,为临床进一步了解支气管扩张与心肺功能的关系提供了新的思路。
原文出处:
Alejandro A Diaz,Laura A Colangelo,Yuka Okajima,et al.Association between Cardiorespiratory Fitness and Bronchiectasis at CT: A Long-term Population-based Study of Healthy Young Adults Aged 18-30 Years in the CARDIA Study.DOI:10.1148/radiol.2021203874
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#扩张#
32
#支气管#
40
学习
75
学习了
73
挺好的
78
挺好的
69