Nat Commun:北京市COVID-19病例基因组监测情况
2020-10-30 haibei MedSci原创
研究人员根据代表性的高频单核苷酸多态性(SNPs),将所有测序基因组分为7个簇。基因组比较显示,与武汉暴露组和本地传播组相比,海外输入组的基因组多样性较高,表明在全球传播过程中基因组持续进化。
2019年冠状病毒病(COVID-19)是由严重急性呼吸道综合征冠状病毒2(SARS-CoV-2)引起的一种新兴疾病。这种呼吸道疾病的主要症状包括咳嗽、发热、呼吸急促,从轻度到重度不等。自2019年12月首次报告病例以来,该病已在235个国家和地区造成超过3400万例感染和超过100万例死亡。
根据新增病例的时空分布,从疫情发展来看,其可以分为两个时期。2019年底至2020年2月,疫情主要在中国境内传播,2月12日为新增病例高峰期。在实施了一系列干预措施后,包括旅行者的常规筛查和隔离、自我隔离和检测、接触限制、社会疏导等措施,中国境内新发感染病例减少,疫情得到良好控制。2月底,欧洲和地中海东部地区开始出现零星病例和疫情。当欧美地区感染人数超过中国时,疫情发展到新阶段。
3月11日,世界卫生组织正式宣布全球爆发疫情,114个国家报告的感染人数超过11.8万人。随着欧美成为疾病爆发的中心,中国开始出现国外的病例输入。于是,中国疾病控制的重点从社区层面的干预转向控制边境和移民。中国对疾病控制的严格衡量就变成了对输入性感染的检测和检疫。通过在机场等入境口岸对入境旅客实施体温测量和实时聚合酶链反应(RT-PCR)检测等筛查措施,成功地将这些输入性病例在当地的进一步传播降到最低。截至5月30日,我国已录得1700多例输入性病例,包括中国旅行者、中国海外居民和外国旅行者(http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml)。

最近,我国研究人员在Nature Communications杂志发文,提供了102例输入性病例的基因组监测数据,占北京总病例的17.2%。其数据表明,北京的所有病例大致可以分为三类:武汉暴露、本地传播和海外输入。
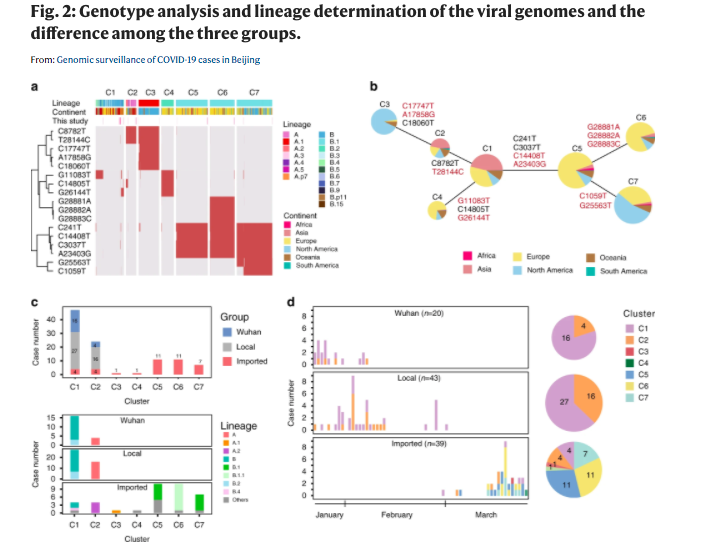
研究人员根据代表性的高频单核苷酸多态性(SNPs),将所有测序基因组分为7个簇。基因组比较显示,与武汉暴露组和本地传播组相比,海外输入组的基因组多样性较高,表明在全球传播过程中基因组持续进化。
输入组表现出区域特异性SNP,而宿主内单核苷酸变异则表现为随机特征,组间无明显差异。
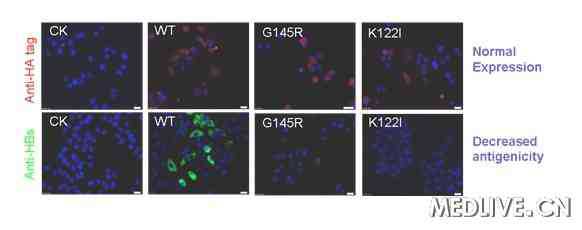
流行病学数据表明,在入境时发现病例并进行强制隔离可能是防止输入病例引发反复爆发的有效途径。值得注意的是,研究人员还发现了一组新的突变。
这些数据意味着SARS-CoV-2基因组可能具有较高的突变容忍度。
原始出处:
Pengcheng Du et al. Genomic surveillance of COVID-19 cases in Beijing. Nature Communications (2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#COMMUN#
33
#监测情况#
44
#Nat#
38
深度学习新冠知识
129
继续学习新内容
108