Brilacidin治疗COVID-19的II期临床试验,计划于下周开始
2021-01-31 Allan MedSci原创
临床阶段生物制药公司Innovation Pharmaceuticals近日宣布,该公司用于治疗COVID-19的Brilacidin的II期临床试验计划于下周开始。
临床阶段生物制药公司Innovation Pharmaceuticals近日宣布,该公司用于治疗COVID-19的Brilacidin的II期临床试验计划于下周开始。

II期随机、安慰剂对照临床试验将招募约120例中重度COVID-19住院患者,患者随机分配至Brilacidin治疗组和安慰剂对照组,每组约有60例患者。该试验的主要终点是根据美国过敏和传染病研究所(NIAID)制定的第29天持续恢复时间,其他终点包括:院内预后、全因死亡率、炎症相关生物标志物的测定、SARS-CoV-2病毒载量的变化。
该公司认为,Brilacidin具有巨大的前景,有望帮助解决COVID-19全球大流行。
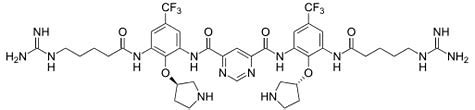
Brilacidin的抗病毒作用机制是通过破坏病毒膜完整性直接攻击冠状病毒。这表明,即使病毒产生突变,Brilacidin仍能攻击病毒。Innovation公司期待着开始其临床试验,以进一步评估Brilacidin的COVID-19治疗潜力。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#acid#
35
#I期临床试验#
28
#CID#
0
#II期临床试验#
37
#II期临床#
34
#I期临床#
0