微创主动脉瓣膜完成上市后首例植入 比国内现有产品优惠30%以上
2019-08-29 佚名 医谷
昨日(8月28日),微创旗下子公司微创心通医疗自主研发的VitaFlow®活力流经导管主动脉瓣膜系统在上海复旦大学附属中山医院完成了上市后首例植入,该手术由中国科学院院士、复旦大学附属中山医院心内科主任葛均波主刀,为一位70岁高龄的男性患者成功植入了VitaFlow主动脉瓣膜。
昨日(8月28日),微创旗下子公司微创心通医疗自主研发的VitaFlow活力流经导管主动脉瓣膜系统在上海复旦大学附属中山医院完成了上市后首例植入,该手术由中国科学院院士、复旦大学附属中山医院心内科主任葛均波主刀,为一位70岁高龄的男性患者成功植入了VitaFlow主动脉瓣膜。
据了解,VitaFlow瓣膜系统由主动脉瓣膜、输送系统、装载工具、瓣膜球囊扩张导管和导管鞘套件组成。其通过创新性的双层“裙边”设计能够更有效的降低术后瓣周漏,混合密度网格镍钛支架,使瓣膜能够有效撑开钙化瓣叶,且在释放过程中具有优异的同轴和定位性能;大网孔设计,则为冠状动脉的介入治疗预留了空间。同时,该产品采用电动输送系统,方便术者在释放瓣膜的同时操控导丝,兼顾了柔顺性和强度的管材设计,既降低了血管并发症发生率,又保证了释放的稳定与精准。产品还搭配微创心通自主研发的球囊扩张导管和导管鞘套件,进一步为医生提供了全面的整体治疗方案,提高了手术的安全性和有效性。
2016年,VitaFlow瓣膜系统通过了原CFDA的创新医疗器械特别审批申请,进入了特别审批程序“绿色通道”,今年7月,其获得国家药品监督管理局颁发的注册证,这也是国内首个获准上市的自膨胀式牛心包生物瓣膜。
另据微创方面透露,VitaFlow瓣膜系统的价格预计将比国内市场上的现有产品优惠30%以上。
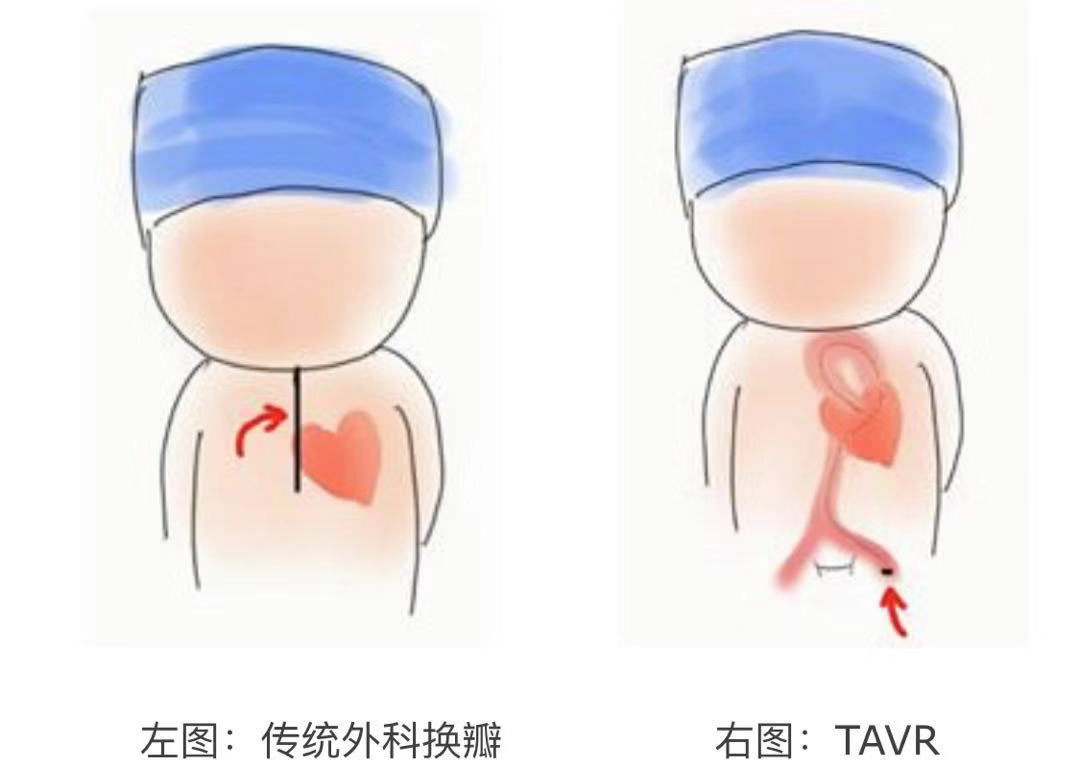
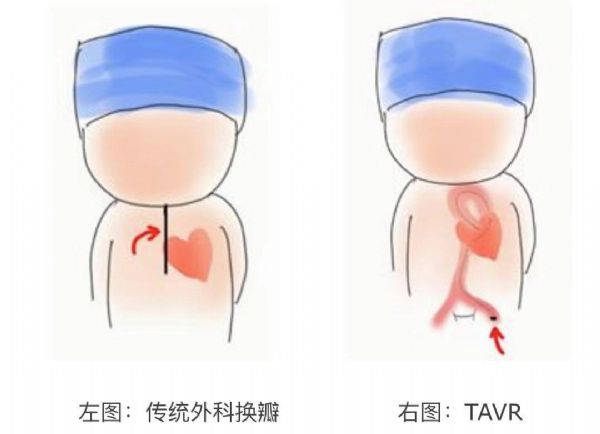
主动脉瓣狭窄是老年人中最常见也是最严重的瓣膜病之一,随着患者年龄的增长,患病率显着升高。在西方国家,主动脉瓣狭窄在65岁及以上的人群中发病率约为2%,在85岁及以上的人群中发病率约为4%,若不及时干预,患者中位生存期为2至3年。经导管主动脉瓣置换术(Transcatheter aortic valve replacement,TAVR)作为近年来用于临床的介入治疗手术,为那些不能耐受外科主动脉瓣置换术的高危重症主动脉瓣狭窄患者提供了较为理想的替代治疗方案。
从国外TAVR临床应用路径来看,专家认为,TAVR对治疗无法接受外科换瓣病人的地位已无法撼动;对高危外科换瓣的病人,虽然指南仍建议TAVR和SAVR地位相同,但实际临床上逐步倾向TAVR;对中危外科换瓣的病人,美国2017年的瓣膜疾病治疗指南建议,外科主动脉瓣膜置换术(surgical aortic valve replacement,SAVR)是一级推荐,TAVR是IIa级推荐。欧洲的瓣膜疾病治疗指南则建议,中危外科换瓣的病人若年纪大(≧75岁)且可以经由股动脉入路执行TAVR,则可以使用TAVR。因此,也可以看出,TAVR越来越受肯定,临床地位日趋重要。
目前全球已有60多个国家、约35万例患者植入TAVR产品。随着人口老龄化的不断加剧和适应证的拓展,预计未来10年内全球TAVR手术量将增长4倍,预计2021年TAVR全球市场超过50亿美金。
TAVR在欧美的发展较为成熟,欧洲地区作为TAVR领域最大的细分市场之一,2017 年占据了全球近一半的市场份额。在美国,TAVR同样发展迅猛。据统计,美国进行TAVR手术的医院数目已由2013年的252家增长至2018年的642家。2018年,美国TAVR手术数量达到6万台次之多。
在中国市场,虽然应用TAVR治疗起步较晚,但伴随着总计约有280万重度主动脉瓣狭窄患者群体,TAVR发展速度非常迅猛,自2010年首例TAVR手术以来,现在已有20余个省市的100多家医院开展了近2000例TAVR手术,市场空间巨大。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#微创#
27
#主动脉瓣#
29
#主动脉#
33
#植入#
39
#瓣膜#
24