第十七届中国介入心脏病学大会(CIT2019)|高鑫:经皮肺动脉血管成形术围术期管理
2019-04-03 lily MedSci原创
经皮肺动脉血管成形术围术期管理血管成形术是指使狭窄的血管恢复原来形状的一种方法,主要用于冠心病、心肌梗死的治疗。阜外心血管医院高鑫教授在CT2019讲解了经皮肺动脉血管成形术围术期管理应重点注意的问题。一、各项检查术前常规检查如下,但要特别重视肺动脉CTA。二、抗凝管理华法林:目标INR 2.0-3.0维生素K拮抗剂:有多重药物-药物和药物-食物相互作用,因此在不同病人剂量差异较大,需频繁检测使I
血管成形术是指使狭窄的血管恢复原来形状的一种方法,主要用于冠心病、心肌梗死的治疗。
阜外心血管医院高鑫教授在CT2019讲解了经皮肺动脉血管成形术围术期管理应重点注意的问题。
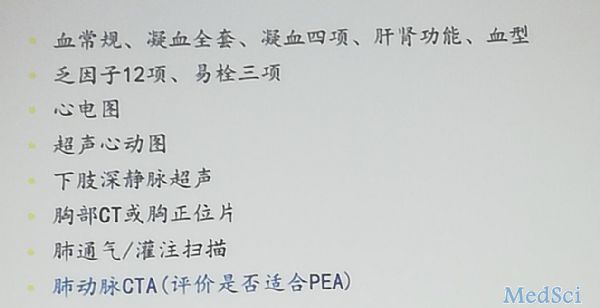
一、各项检查
术前常规检查如下,但要特别重视肺动脉CTA。
二、抗凝管理
华法林:目标INR 2.0-3.0
维生素K拮抗剂:有多重药物-药物和药物-食物相互作用,因此在不同病人剂量差异较大,需频繁检测使INR 2.0-3.0。
新型口服抗凝药应列为VTE的一线抗凝治疗,AT10推荐由于华法林。常规选用利伐沙班,原应用华法林的患者入院侧INR,如小于1.8-2.0,则启用利伐沙班20mg qd。大动脉炎肺动脉受累患者围术期应用利伐沙班,术后考虑用阿司匹林及他汀类药物维持。
三、血糖管理
对大多数患者来说血糖应维持在7.8mol/l-10.0mol/l。在能安全达标的前提下餐前血糖应尽可能小于7.8mol/l,且随机血糖小于10mol/l。
四、血压血脂管理
抗高血压治疗:血压应控制在140/90mm Hg以内
调脂治疗:治疗目标为LDL-C低于2.60mol/l;对于极高危患者LDL-C应低于1.8mol/l
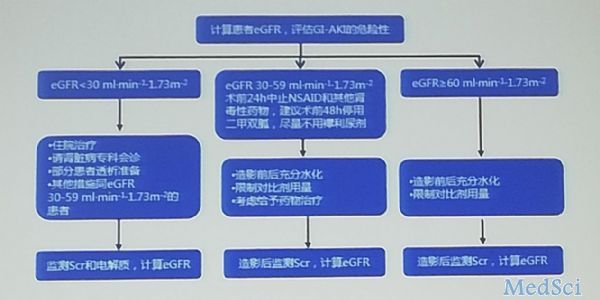
五、预防对比剂致急性肾损伤
包括:基础肾功能评估;术前危险分层;水化治疗;控制对比剂的用量
六、含碘造影剂患者的处理流程
七、具体对比剂使用
肾功能正常患者:对比剂剂量控制在4-6ml/kg以内,总量不宜超过300-400ml,并予以充分水化。
慢性肾病患者可根据肌酐清除率计算对比剂使用剂量,限定最大对比剂使用剂量。
推荐的水化方法:造影前至造影后,持续静脉滴注生理盐水1.0-1.5ml/kg/h,保持尿量75-125ml/h。
八、合并心力衰竭的处理
合并CHF者行BPA的围手术期死亡风险增加,必须干预。BPA前过渡性治疗,降低肺动脉阻力、改善血流动力学、纠正右心衰,以减少BPA围术期并发症风险。不利之处在于利尿治疗会同时降低PAMP,会消除可能同时存在的毛细血管后肺高压。
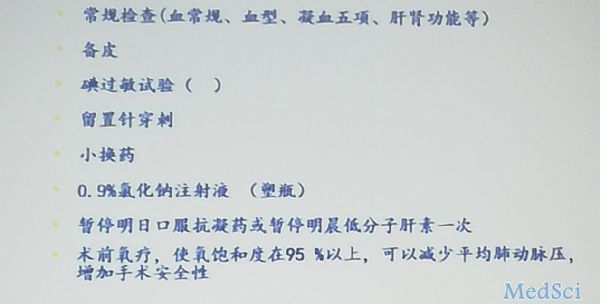
九、术前准备
简要介绍手术方法,消除患者紧张情绪,术前保证良好的状态。
常规术前操作包如下
十、术后
返回病房后,即刻监测生命体征。
十一、术后次日复查
血常规;B型钠酸胎;D-二聚体;心梗三项;电解质+肝功+肾功+心肌酶谱+血糖;远达正侧位胸片;动脉血气分析。
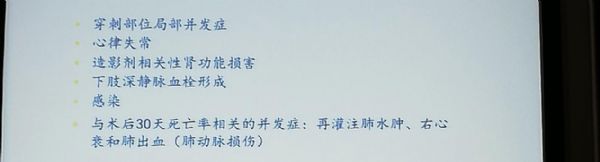
十二、术后并发症
文献表明并发症发生率36.3%,多于其他介入治疗。原因包括介入治疗的血管数量多、血管随呼吸运动不能避免,肺血管容易受损。
并发症主要包括:
重点介绍发病率很高的几种并发症:
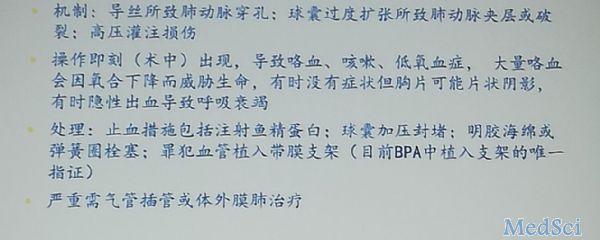
1、急性肺出血
术后即可发生,发生率高达30%。
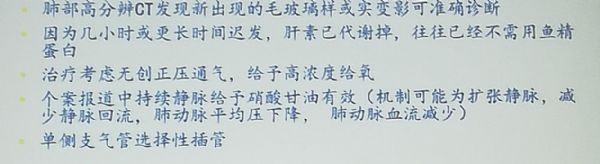
2、亚急性肺出血
往往是由于肺动脉扩张,后破裂后缓慢渗出所致。
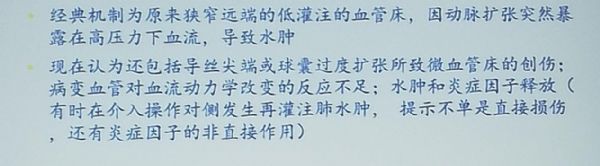
3、再灌注肺水肿
也是外科肺动脉血栓内膜剥脱术的主要并发症,早期BPA的文献较常见,但近期文献发生率减少,提示岁经验的积累其发生率下降,主要为技术原因。
十三、治疗
无创正压通气,气管插管呼吸机辅助呼吸,必要对ECMO类固醇激素的疗效仍需证实
输注白蛋白,提升胶体渗透压,后在辅助利尿。以上措施认为对预防BPA后肺水肿无效。
十四、预防
危险因素包括:平均肺动脉压的升高,左右和住肺动脉直径指数升高,球囊动脉直径比升高,远端扩张后压力仍然升高。
最新文献2019回归分析表明,完全闭塞性病变是操作相关并发症的唯一的危险因素
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#心脏病学#
34
#CIT#
32
#介入心脏病学#
37
#成形术#
20
#动脉血#
26
#血管成形术#
27
#围术期#
37
#围术期管理#
32