J Thorac Oncol:针对原发性肺癌的低剂量CT(LDCT)筛查对后续发生脑转移(BM)风险的影响。
2021-06-03 yd2015 MedSci原创
基于大规模人群研究发现,采用低剂量CT(LDCT)筛查早期发现原发性肺癌(PLC),可降低PLC诊断后发生脑转移(BM)的风险。
脑转移(BM)是原发性肺癌最常见的转移部位之一。约10%患者初始诊断时伴有BM,而40%患者在疾病过程中会出现BM。肺癌患者伴有BM通常提示预后较差。但是研究表明,对于BM如果能够控制症状,是可以改善其预后。因此,对于BM的早期诊断显得尤其重要。2011年,国际肺癌筛查研究(NLST)表明低剂量CT (LDCT)筛查通过对增加早期肺癌的诊断从而可以降低原发性肺癌约20%的死亡风险。肺癌长期生存患者可能增加脑转移瘤的发生几率。但是,目前还不清楚,LDCT筛查是否可影响肺癌患者发生脑转移的风险。基于此,国外研究团队利用NLST数据库,旨在探讨LDCT筛查对诊断肺癌后患者发生脑转移的影响。近期,研究成果发表在Journal of Thoracic Oncology杂志上。
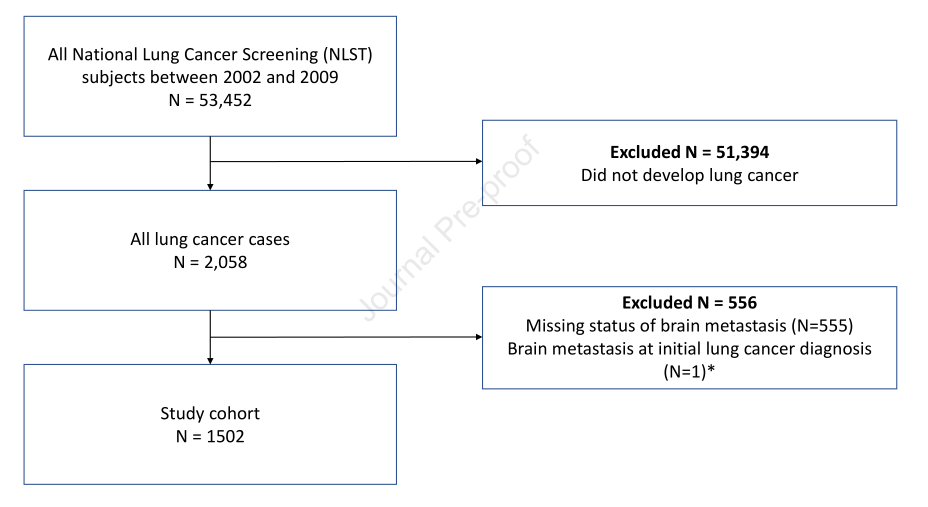
研究利用NLST数据库中纳入2002至2009年诊断肺癌的1502例患者,随访观察BM的发生。1502例患者中,41.4%患者是通过LDCT筛查发现原发性肺癌的,58.6%患者是通过其他方式发现原发性肺癌的,如胸部X线or临床症状等。中位随访2.5年,1502例原发性肺癌患者中有143例(9.5%)出现脑转移。大约四分之一的BM患者诊断时为I期患者。对于非小细胞肺癌(NSCLC)患者,I期患者中LDCT筛查出现BM几率为32.4% (11 out 34),而没有LDCT筛查的为22.2% (14 out of 63)。而小细胞肺癌(SCLC)患者出现BM为II期或以上的患者。
研究概况
相对于其他方式发现的肺癌患者,LDCT筛查发现的肺癌患者3年BM发生率更低(6.5% vs 11.9%,HR=0.53(经相关因素调整后), 95% CI 0.36-0.78, P=0.001)。亚组分析发现,对早期原发性肺癌(I-III期)患者,LDCT筛查可以降低BM发生风险(HR 0.47, 95%CI 0.29-0.75, p=0.002)。同样,对于I-II期患者,LDCT筛查可以降低BM发生风险(HR 0.35, 95%CI 0.18-0.68, p=0.002)。对于手术治疗的患者,LDCT筛查也可以降低BM发生风险(HR 0.37, 95%CI 0.21-0.68, p=0.001)。
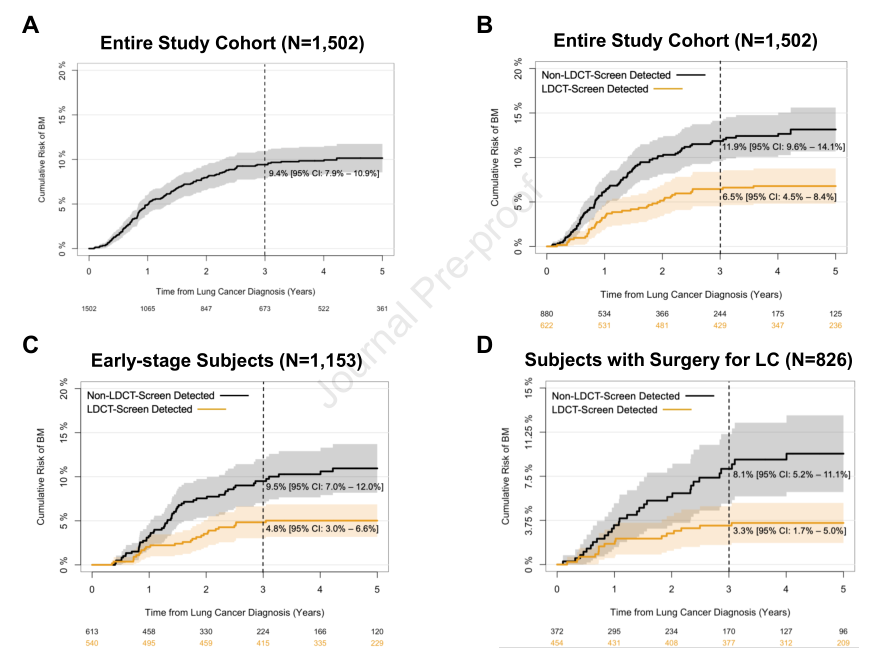
不同组发生BM的风险1

不同组发生BM的风险2
敏感性分析发现,相对于胸部X线,LDCT可以降低BM发生风险(HR = 0.63, CI 0.45 – 0.89, p=0.008)。因为研究发现I期患者出现BM几率较高,研究者把其分为BM组和非BM组,探索其结节的特征区别。研究发现,发生BM的患者结节生长速度明显增快(6.4 mm vs. 3.6 mm/每月)。
综上,基于大规模人群研究发现,采用低剂量CT(LDCT)筛查早期发现原发性肺癌(PLC),可降低PLC诊断后发生脑转移(BM)的风险。
原始出处:
Su CC, Wu JT, Neal JW, et al. Impact of Low-Dose CT Screening for Primary Lung Cancer on Subsequent Risk of Brain Metastasis, Journal of Thoracic Oncology (2021), doi: https://doi.org/10.1016/j.jtho.2021.05.010.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#THORAC#
37
#Oncol#
38
#原发性#
34
#LDCT#
35
#低剂量CT#
57
#低剂量#
31
#原发性肺癌#
31
实用性
62
JTO上有很多不错的好文章,谢谢梅斯及时上新
48
谢谢梅斯分享这么多精彩信息
58