J Clin Oncol:用MRI替代CT以及拉长复查间隔对I期精原细胞瘤患者的长期预后无不良影响
2022-03-22 Nebula MedSci原创
MRI可以减少I期精原细胞瘤患者受到的辐射量;而且减少扫描次数对长期预后没有不良影响
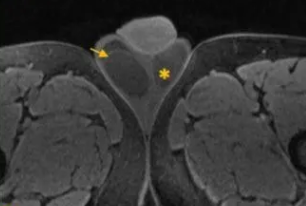
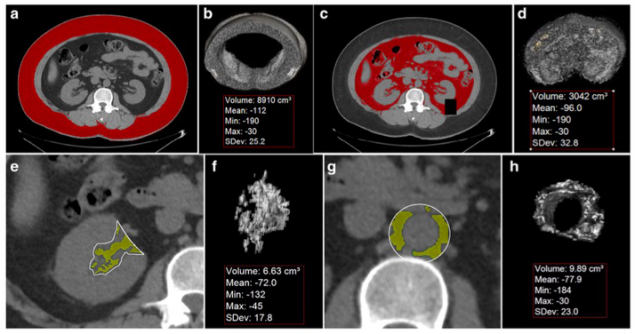
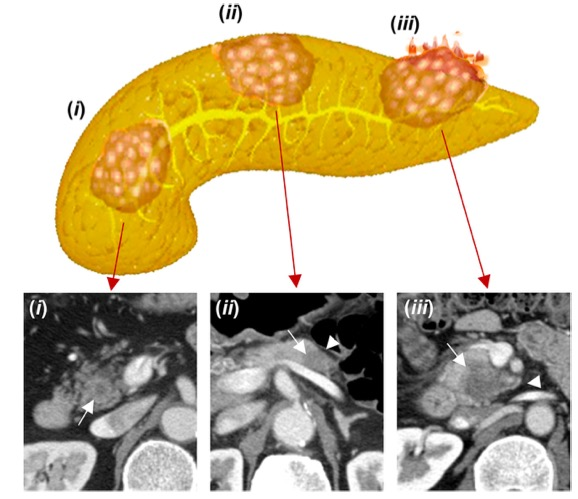
在临床上,约一半的睾丸肿瘤是精原细胞瘤。I 期精原细胞瘤睾丸切除术后的存活率几乎是100%。虽然辅助放疗可有效地减少复发,但由于长期毒性的担忧和替代疗法的出现,放疗的使用率在最近几十年急剧下降。CT 监测是精原细胞瘤的一项国际医疗标准,可避免过度辅助治疗。特别是对于年轻患者,尽量减少放疗是至关重要的。
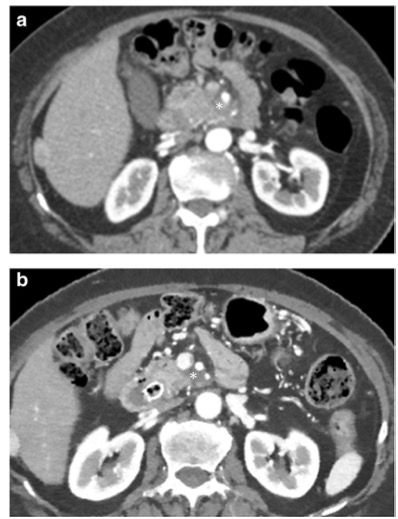
TRISST试验是一项非劣效性的 3 期阶乘试验,旨在评估采用核磁共振(MRI)检查或减少扫描频次是否能不增加晚期复发率。纳入了进行了睾丸切除术且无辅助治疗计划的 I 期精原细胞瘤患者。受试患者被随机成四组,分别接受7次CT扫描(第6、12、18、24、36、48和60个月时)、7次MRI扫描(相同时间)、3次CT扫描(6、18和36个月)或3次MRI扫描(相同时间)。主要终点是 IIC 期复发(>5cm)的6年发生率。次要终点包括复发≥3cm、无病生存期和总生存期。
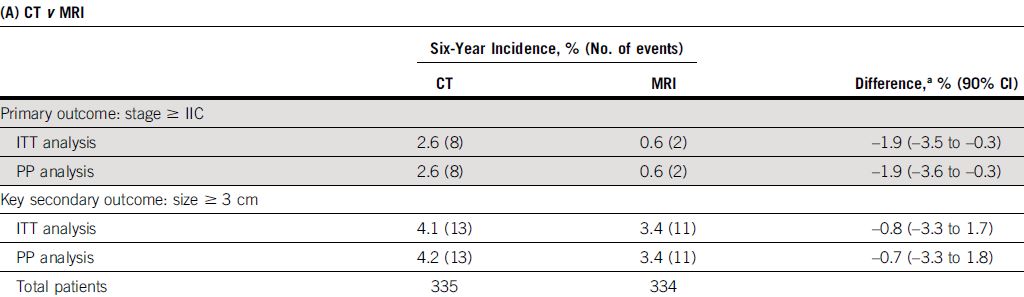
MRI vs CT扫描的6年晚期复发率
2008年至2014年期间,共招募了669位患者,平均肿瘤大小是2.9cm,358例(54%)是低风险(<4cm,无睾丸网侵犯)。中位随访了72个月,82位(12%)患者复发。≥IIC期的复发很少(10例)。虽然在统计学上非劣效性,但接受三次扫描的患者的≥IIC期的复发(9例,2.8%)多于接受7次扫描(1次,0.3%):绝对发生率增加了2.5%。只有4/9的患者可能通过7次扫描更早地被发现复发。
3次 vs 7次扫描的6年晚期复发率
此外,分析结果显示与CT相比,MRI表现亦非劣效性;MRI检出的复发事件更少(2例[0.6%] vs 8例[2.6%]),绝对发生率降低了1.9%。按方案分析证实非劣效性。5年生存率为99%,无肿瘤相关死亡病例。
总之,无论采用的监测方法或频次如何,监测都是一种安全且有效的管理方法,精原细胞瘤晚期复发很少见,挽救性治疗效果很好,患者预后很好。MRI可以减少辐射量;而且减少扫描次数对长期预后没有不良影响。
原始出处:
Johnathan K. Joffe, et al. Imaging Modality and Frequency in Surveillance of Stage I Seminoma Testicular Cancer: Results From a Randomized, Phase III, Noninferiority Trial (TRISST). J Clin Oncol. March 15, 2022. https://ascopubs.org/doi/full/10.1200/JCO.21.01199
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#长期预后#
47
#Oncol#
43
#细胞瘤#
38
#精原细胞瘤#
43