近日,默沙东、欧洲癌症研究与治疗组织(EORTC)和欧洲胸腔肿瘤学平台(ETOP)公布了其关键III期临床试验KEYNOTE-091(又称EORTC-1416-LCG/ETOP-8-15-PEARLS)的研究数据。该研究旨在评估PD-1抑制剂帕博利珠单抗对比安慰剂,联合或不联合辅助化疗,用于IB 期(T≥4 cm)至IIIA期非小细胞肺癌(NSCLC)患者手术切除(肺叶切除术或全肺切除术)后辅助治疗的疗效。KEYNOTE-091研究数据在欧洲肿瘤内科学会(ESMO)线上全体会议(Virtual Plenary)上公布。
根据世界卫生组织数据显示,中国2020年肺癌新发病例约为81.6万,死亡病例约为71.5万。研究显示,非小细胞肺癌患者即使接受了肿瘤完全切除术,仍存在术后复发、转移和再发第二原发肺癌的风险,超过50%的肿瘤复发或转移发生于术后前2年-。术后辅助治疗是早中期非小细胞肺癌肿瘤完全切除术后减少复发、延长生存和改善生活质量的重要治疗组成,可以为患者带来更多临床获益。
KEYNOTE-091是一项随机、三盲、III期临床试验,旨在评估帕博利珠单抗、与安慰剂对照,联合或不联合辅助化疗作为手术切除(肺叶切除术或全肺切除术)后IB-IIIA期(AJCC第7版TNM分期标准)非小细胞肺癌患者辅助治疗的有效性和安全性差异。研究的主要终点是总体人群和PD-L1高表达(TPS ≥50%)人群的无病生存期(DFS);研究的次要终点包括总生存期(OS)、肺癌特异性生存期(LCSS)。研究共入组了IB-IIIA期,实现R0切除的1177例NSCLC患者,按1:1随机分组接受帕博利珠单抗(每3周1次200mg, 静脉滴注,持续1年或最多给药18次)或安慰剂治疗。
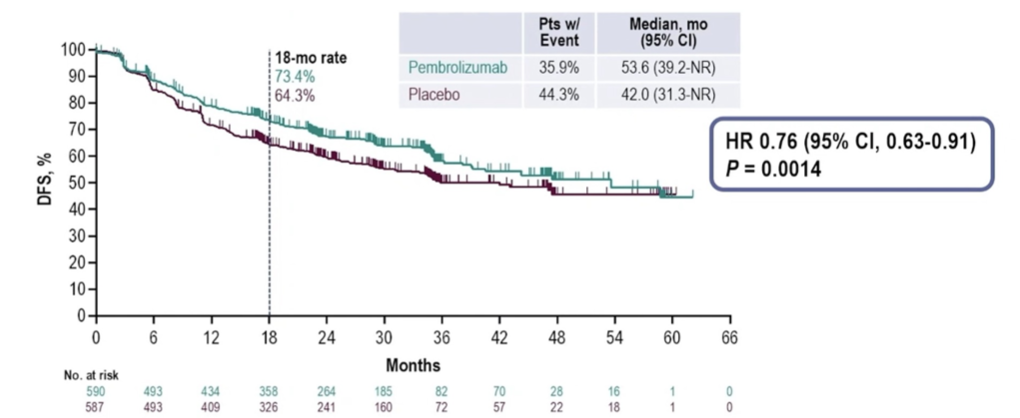
此次发布的KEYNOTE-091期中分析数据显示,KEYNOTE-091到达了双重主要终点之一,即帕博利珠单抗作为IB-IIIA期非小细胞肺癌患者的手术后辅助疗法,相比安慰剂对照,对总体人群(无论PD-L1表达水平)的DFS具有统计学和临床意义上的显著改善。
接受帕博利珠单抗作为辅助治疗的患者中位DFS为53.6个月,与安慰剂对照组(中位DFS42.0个月)的数据相比有将近一年的改善。
同时,患者术后疾病复发或死亡的风险降低了24%(HR=0.76 [95% CI, 0.63-0.91];p=0.0014)。
线上全体大会所公布的数据也意味着,无论PD-L1表达水平,帕博利珠单抗或将成为早期肺癌患者术后辅助治疗的新选择。
截至目前,中国国家药品监督管理局(NMPA)批准的帕博利珠单抗的适应证共有8个,分别覆盖黑色素瘤、肺癌、食管癌、头颈癌、结直肠癌和食管癌。帕博利珠单抗联合或不联合辅助化疗、用于IB至IIIA期非小细胞肺癌(NSCLC)患者术后辅助治疗的适应证尚未获得NMPA批准。
参考资料:
1,IARC. China Fact Sheet (2020).
2,Lou F, Huang J, Sima CS, et al. Patterns of recurrence and second primary lung cancer in early‐stage lung cancer survivors followed with routine computed tomography surveillance[J]. J Thorac Cardiovasc Surg, 2013, 145(1):75‐81; discussion 81‐82. DOI: 10.1016/j. jtcvs. 2012.09.030.
3, 陆舜、吴一龙等 《Ⅰ~ⅢB期非小细胞肺癌完全切除术后辅助治疗指南(2021版)》中华医学杂志2021年4 月27日第101卷第16 期
4, 陆舜、吴一龙等 《Ⅰ~ⅢB期非小细胞肺癌完全切除术后辅助治疗指南(2021版)》中华医学杂志2021年4 月27日第101卷第16 期
5, 此处,DFS定义为从随机化分组到疾病复发及远处转移(包括第二原发性非小细胞肺癌或其他恶性肿瘤)或任何原因导致死亡的时间,以先发生者为准。
6, 此处,LCSS定义为从随机化到由于肺癌所致死亡日期的时间
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#帕博利珠#
45
#非小细胞#
38
#帕博利珠单抗#
58
#III#
39
#研究数据#
48