Clin Cancer Res:ATTRACTION-3研究3年随访生存结果表明nivolumab较化疗改善晚期食管鳞状细胞癌(ESCC)患者预后
2022-03-23 yd2015 网络
研究表明,二线治疗nivolumab(那武利尤单抗)较化疗改善晚期食管鳞状细胞癌(ESCC)患者的预后。
ATTRACTION-3是一项随机、多中心、开放标签的III期临床研究,主要是在既往经治的晚期食管鳞状细胞癌(ESCC)患者中对比PD-1抑制剂nivolumab(那武利尤单抗)和化疗(紫杉醇或多西他赛)治疗的疗效。中位随访17.6个月后,研究报告nivolumab组的中位总生存期(OS)为10.9个月,化疗组的中位总生存期(OS)为8.4个月(风险比[HR], 95%CI, 0.77 [0.62-0.96];p = 0.019)。Nivolumab和化疗组18个月的OS率分别为31%和21%,12个月的无进展生存期(PFS)率分别为12%和7%。因此,nivolumab较化疗明显改善患者的预后。近期,Clin Cancer Res杂志上发表了ATTRACTION-3研究3年随访生存结果。
在2016年1月7日-2017年5月25日期间,590名患者接受了评估,419名患者被随机分配到治疗中:210名患者接受了nivolumab治疗,209名患者接受了化疗。应答可评估人群包括329名患者(nivolumab,n = 171;化疗,n = 158)和安全人群包括417名患者(nivolumab,n = 209;化疗,208例)。
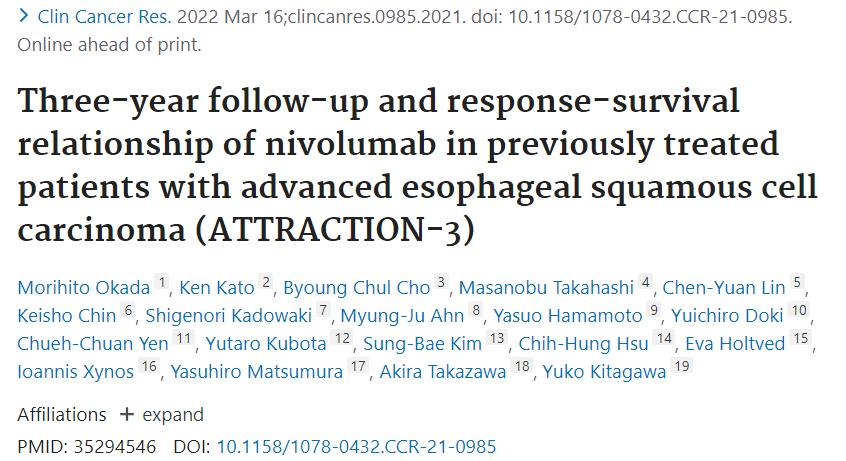
在临床截止时间(2020年5月25日),最短随访时间为36.0个月。Nivolumab组和化疗组的中位OS (95% Cl)分别为10.9(9.13.3)和8.5(7.3 9.9)个月。Nivolumab的死亡风险显著低于化疗组(HR [95% CI], 0.79 [0.64 0.97];p = 0.0264)。总的来说,与化疗组相比,nivolumab组在1年(46.9% vs 34.7%)、2年(20.2% vs 13.5%)和3年(15.3% vs 8.7%)OS率更高。Nivolumab组与化疗组的中位PFS (95% CI)分别为1.7(1.5 2.7)和3.4(3.0 4.2)个月,HR为1.07(0.87 1.33)。与化疗组相比,nivolumab组在1年(11.9% vs 7.2%)、2年(5.4% vs 2.4%)和3年(4.3% vs 1.6%)的PFS率更高。
Nivolumab组与化疗组的的ORR分别为19.3%和21.5%;DCR分别为37.4%和62.7%;中位DOR (95% CI)分别为6.9(5.4 11.1)个月和3.9 (2.8–4.2)个月。

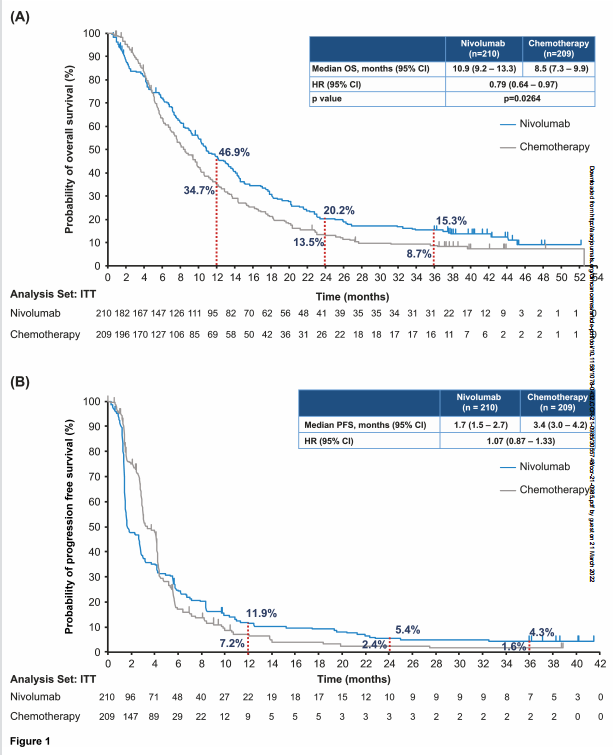
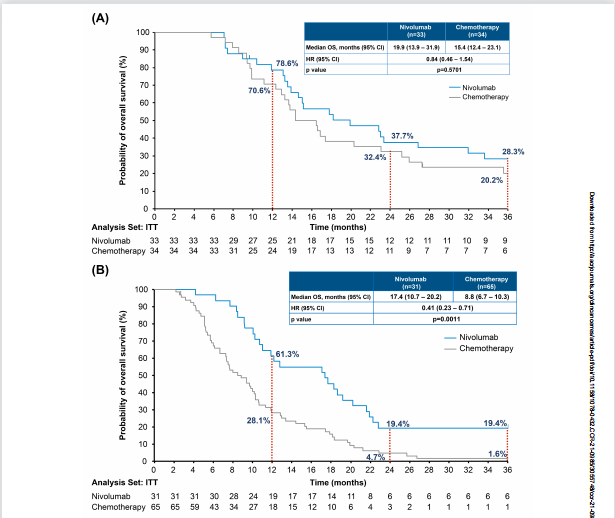
Nivolumab组和化疗组患者获得CR/PR, SD, 和PD的中位OS分别为 19.9 vs. 15.4 个月(HR [95% CI], 0.84 [0.46 1.54]), 17.4 vs. 8.8个月(HR [95% CI], 0.41 [0.23 0.71]),和7.6 vs. 4.2个月(HR [95% CI], 0.59 [0.39 318 0.88])。
停药原因(Nivolumab vs.化疗)为疾病进展[140 (67.0%)vs. 138(66.3%)]、AEs [16 (7.7%) vs. 8(3.8%)]、医生的判断[17 (8.1%)vs. 27(13.0%)]和其他原因[21 (10.0%)vs. 19(9.1%)]。Nivolumab组210例患者中127例(60.5%)接受了后续治疗,化疗组209例患者中118例(56.5%)接受了后续治疗。在nivolumab和化疗组中,大多数患者接受了后续的全身治疗(56.2%对49.8%)。
Nivolumab组有138例(66.0%)患者报告了任何级别的TRAE,化疗组有198例(95.2%)患者报告了任何级别的TRAE,其中≧3级TRAE分别为40例(19.1%)和133例(63.9%)。Nivolumab组209例患者中有35例(16.7%)报告了严重TRAE,化疗组208例患者中有47例(22.6%)报告了严重TRAE。
综上,研究表明,二线治疗nivolumab(那武利尤单抗)较化疗改善晚期食管鳞状细胞癌(ESCC)患者的预后。
原始出处:
Okada M, Kato K, Cho BC, Takahashi M, Lin CY, Chin K, Kadowaki S, Ahn MJ, Hamamoto Y, Doki Y, Yen CC, Kubota Y, Kim SB, Hsu CH, Holtved E, Xynos I, Matsumura Y, Takazawa A, Kitagawa Y. Three-year follow-up and response-survival relationship of nivolumab in previously treated patients with advanced esophageal squamous cell carcinoma (ATTRACTION-3). Clin Cancer Res. 2022 Mar 16:clincanres.0985.2021. doi: 10.1158/1078-0432.CCR-21-0985. Epub ahead of print. PMID: 35294546.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#细胞癌#
34
#Tract#
33
#SCC#
45
#mAb#
26
#患者预后#
35
#TTR#
27
#TRA#
22
#NIV#
48
学习
32
#食管鳞状细胞癌#
46