PLOS MED:不论心血管状况,不论运动强度,锻炼都能降低心血管死亡率!
2022-01-05 MedSci原创 MedSci原创
既往的研究已经证实,中等强度的体力活动(MVPA)与非传染性疾病和死亡率的风险降低密切相关。
既往的研究已经证实,中等强度的体力活动(MVPA)与非传染性疾病和死亡率的风险降低密切相关。心血管健康状况可能影响MVPA的益处。
为了比较健康人、心血管危险因素(CVRF)水平较高的人和心血管疾病(CVD)之间MVPA与发生的主要不良心血管事件(MACE)和死亡率的关系,来自荷兰奈梅亨的拉德布德健康科学研究所的专家开展了相关研究,结果发表在PLOS Medicine杂志上。
研究人员在荷兰北部3个省进行了一项队列研究,在2006至2018年间收集了数据,中位随访时间为6.8年(5.7-7.9)。生命线队列研究的总共142493名参与者在基线时被分层为(1)健康;(2)CVRF;或(3)CVD。根据自我报告的MVPA量,个人被分为 "不活跃 "和最不活跃(Q1)到最活跃(Q4)四个四分位数。主要结果是随访期间发生的MACE和全因死亡率的综合。
总的来说,健康人的事件发生率为2.2%(2485/112018),CVRF患者为7.9%(2214/27982),CVD患者为40.9%(1019/2493)。健康人(P=0.36)和CVRF患者(P=0.86)的MVPA与全因死亡率或MACE之间没有发现线性关系,但CVD患者有线性关系(P=0.04)。
与不活动的人相比,健康人随着MVPA升高,与不运动的人群风险分别降低19%、21%、28%与24%(HR=0.81,0.71,0.72,0.76)。在有CVRF的人中,与不活动的人相比,MVPA Q1至Q4则分别降低31%、34%、36%、31%(HR=0.69、0.66、0.64和0.69)。
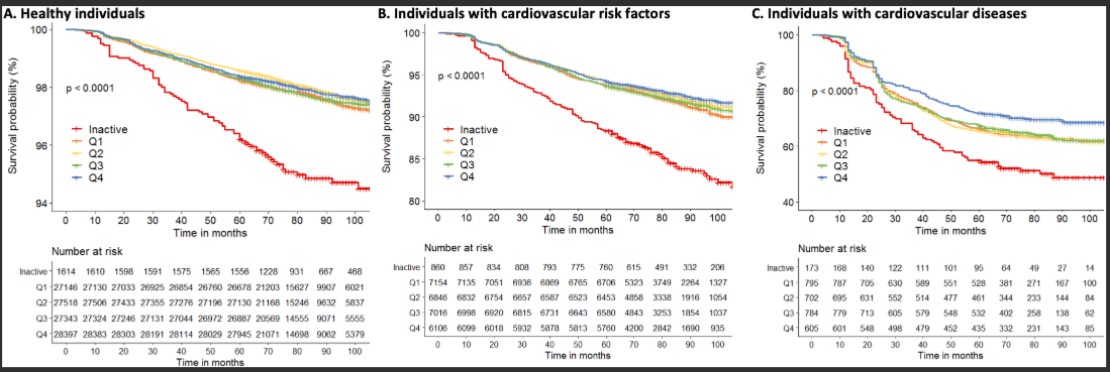
随访期间总MVPA四分位数的全因死亡率和MACE的Kaplan-Meier曲线
最后,在CVD患者中,与非活动者相比,风险降低20%、18%、26%、30%(HR=0.80、0.82、0.74和0.70)。其中,休闲性MVPA与健康益处最大,非休闲MVPA对健康益处很小,而职业性MVPA对健康没有益处。
综上,MVPA有利于减少不良后果,但这种关联的形状取决于心血管健康状况。但CVD患者表现出一种线性关系,表明随着MVPA量的增加,风险不断降低。因此,应鼓励心血管疾病患者在MVPA方面 "多多益善"。
参考文献:
Dose–response association between moderate to vigorous physical activity and incident morbidity and mortality for individuals with a different cardiovascular health status: A cohort study among 142,493 adults from the Netherlands. https://doi.org/10.1371/journal.pmed.1003845
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#运动强度#
46
#心血管死亡率#
40
#心血管死亡#
31
#Med#
0
生命在于运动
54