JACC:北大研究发现长期累积高收缩压、脉压会导致痴呆升高,舒张压则正好相反!
2022-04-08 网络 网络
在年龄≥50岁的认知健康成人中,长期累积血压与随后的认知能力下降、痴呆风险和全因死亡率有关。
根据国际阿尔茨海默病协会的统计,全世界有超过5500万人患有痴呆,到2030年这一数字将上升到7800万。同时,痴呆已成为全球第七大死亡原因。鉴于缺乏有效的治疗方法,确定可改变的风险因素对于延迟发病或减少痴呆症的风险具有重要意义。
几十年来,高血压一直是痴呆症相关研究的一个主要焦点。证据表明,血压升高与认知能力下降和老年痴呆症的发生之间存在关联。然而,很少有研究考虑到长期累积血压暴露影响。
为了测试长期累积血压是否与随后的认知能力下降、痴呆症和认知健康成人的全因死亡率独立相关,来自北京大学临床研究所的专家开展了相关研究,结果发表在JACC杂志上。
本研究使用了来自HRS(健康与退休研究)和ELSA(英国老龄化纵向研究)的数据。累积血压是用ELSA的第0波(1998-1999年)至第4波(2008-2009年)和HRS的第8波(2006-2007年)至第10波(2010-2011年)的测量值计算的曲线下面积。结果包括认知能力下降,发生痴呆,和全因死亡率。
ELSA和HRS中共有7566和9294名参与者(44.8%和40.2%为男性,中位年龄分别为62.0岁[IQR:55.0-70.0岁]和65.0岁[IQR:58.0-72.0岁])。中位随访时间分别为8.0年(IQR:4.0-8.0年)和8.0年(IQR:6.0-8.0年)。累积收缩压和脉压的升高与认知能力的加速下降(两者的P<0.001)、痴呆风险的升高(两者的P<0.001)和全因死亡率(两者的P<0.001)独立相关,而舒张压则有明显的反向关系。强烈的剂量反应关系被确认,2个队列的结果相似。
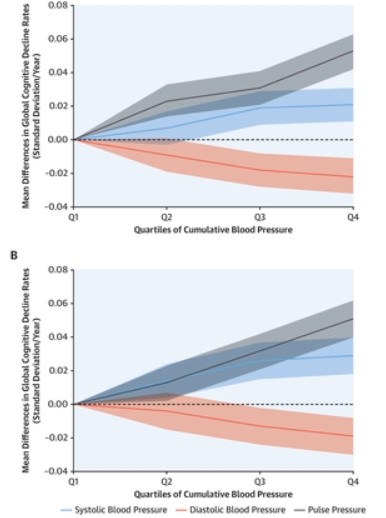
两个独立队列中累积血压认知能力下降率的平均差异
此外, 在两个队列中,仅对累积DBP观察到一致的非线性剂量-反应模式(ELSA的非线性P=0.042,HRS的非线性P=0.017),而在ELSA中仅对累积PP观察到明显的非线性模式。
在年龄≥50岁的认知健康成人中,长期累积血压与随后的认知能力下降、痴呆风险和全因死亡率有关。需要努力控制长期收缩压和脉压,并保持足够的舒张压。
参考文献:
Association of Cumulative Blood Pressure With Cognitive Decline, Dementia, and Mortality. J Am Coll Cardiol. 2022 Apr, 79 (14) 1321–1335
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#收缩压#
48
#JACC#
39
#研究发现#
36
#舒张压#
49
#ACC#
32
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
25