Movement disorders:磷酸化tau181,对鉴别轻度认知障碍和痴呆有何意义?
2022-06-20 Freeman MedSci原创
pTau181与基线或重复测量的认知衰退增加无关。
阿尔茨海默病(AD)和路易体痴呆(DLB)是两种最常见的神经退行性痴呆原因,在英国脑库的研究中,这两种疾病占79%的病例。这两种疾病都有轻度认知障碍(MCI)的前驱症状,曾有报道,与MCI-AD相比,带路易体的MCI(MCI-LB)的衰退速度更快,向痴呆的转化率更高,这与有证据表明在痴呆阶段,DLB患者与AD相比,衰退速度更快,生存时间缩短。
图1: 论文封面图
英国的一项大型脑库研究和前瞻性临床审查报告指出,额外的神经退行性共病变与转化为痴呆的20倍增长有关,另一份来自大型前瞻性尸检系列的报告还发现,LB疾病是这种加速衰退的一个有效的个人层面的因素。
脑脊液(CSF)中Aβ42的减少是AD的一个标志,预示着DLB的快速衰退。其他工作报告说,这种多种病症在MCI阶段已经存在,这使得MCI-DLB患者中存在的AD病症会加速衰退是可信的。
最近,基于血液的识别AD的生物标志物已被报道,特别是血浆中磷酸化tau的测量。人类tau蛋白苏氨酸181处的磷酸化tau(pTau181)已显示出检测AD的效用,其性能与CSF生物标志物和正电子发射断层扫描(PET)tau相当,并与AD病理学的尸检评估相验证。pTau181的升高不仅可以追踪tau病理学,还可以追踪早期淀粉质沉积。 pTau181还可以检测临床前AD,并预测纵向下降和从MCI到AD痴呆的转换。
关于这些血浆生物标志物在DLB中的应用,目前还不太清楚。一项对35名路易体痴呆患者(30名DLB和5名PDD)的研究发现,pTau181似乎是一个有用的AD共同病理标志物,因为它与CSF测量的AD和PET tau相关,并预测PET tau状态。似乎没有研究报告MCI-LB的情况。
一个关键问题是这种生物标志物是否能促进识别DLB/MCI-LB中常见的AD共病症,从而帮助预测有更快衰退风险的个体。pTau181可能能够识别共存的AD病例,并能够评估其纵向进展。
因此,在MCI-LB和MCI-AD中进行了一项前瞻性的纵向研究,在基线上测量pTau181,并进行年度跟踪审查。
他们假设,那些基线pTau181水平与AD共病学存在一致的可能的MCILB患者会有更快的衰退,pTau181不会区分可能的MCI-LB和MCI-AD,但在区分可能的MCI-LB和对照组方面会显示出准确性。他们还报告了重复测量pTau181的一组参与者和那些可能存在MCI-LB的参与者。
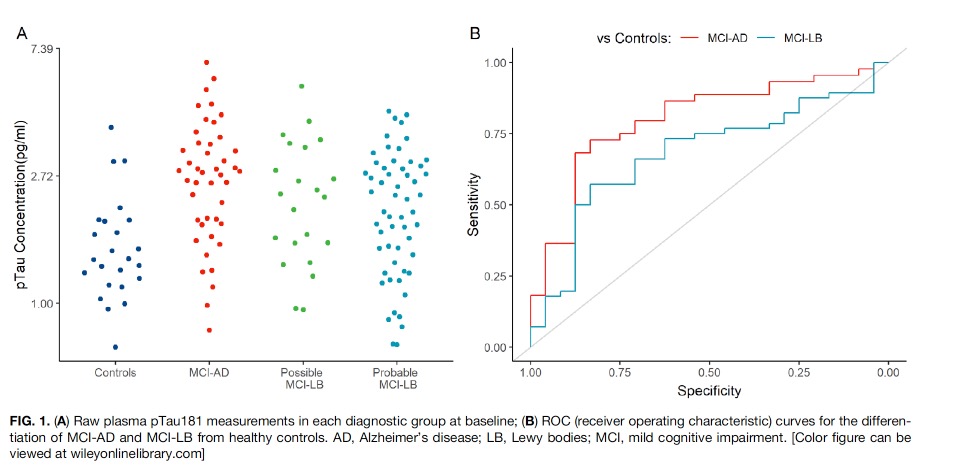
图2:论文结果图
对146名受试者(56名可能的MCI-LB,22名可能的MCI-LB,44名MCI-AD,和24名对照组)进行了长达5.7年的调查。
与对照组相比,可能的MCI-LB的pTau181水平明显较高(平均增加22.2%),而与MCI-AD相比则明显较低(平均下降24.4%)。
pTau181在区分可能的MCI-LB和对照组方面的接收操作特征分析显示,曲线下面积(AUC)为0.68(特异性83%,敏感性57%);
在区分MCI-AD和健康对照组方面,AUC为0.8(特异性83.3%,敏感性72.7%)。
pTau181与MCI-AD的认知能力下降有关联,但在MCI-LB中没有。在一个有重复样本的子集中,血浆pTau181每随访一年有3%的不明显的增加。pTau181的变化率在不同的诊断亚组中没有明显差异。
该研究的重要意义在于发现了:pTau181与基线或重复pTau181测量的认知衰退增加无关。而pTau181部分区分了probable MCI-LB vs control;以及MCI-AD vs control,但对区分可能的MCI-LB与MCI-AD没有帮助。
原文出处:
Thomas AJ, Hamilton CA, Heslegrave A, et al. A Longitudinal Study of Plasma pTau181 in Mild Cognitive Impairment with Lewy Bodies and Alzheimer’s Disease. _Movement Disorders_. Published online March 23, 2022:mds.28994. doi:[10.1002/mds.28994](https://doi.org/10.1002/mds.28994)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




















#Disord#
67
#Dis#
46
#disorder#
53
#disorders#
37
#ERS#
53
#Tau#
0
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
36