Nature子刊:能杀死癌细胞的“铁死亡”疗法是怎么一回事?
2016-11-28 药明康德“学术经纬” 药明康德“学术经纬”微信号
细胞有很多种死亡方式,包括凋亡、自噬和坏死。近年来,“铁死亡”(ferroptosis)作为一种新的细胞坏死方式逐渐进入了人们的眼帘。不同于通常的细胞坏死,铁死亡是一种受调控的坏死过程。铁死亡是由于膜脂修复酶——谷胱甘肽过氧化物酶(GPX4)失效,造成膜脂上活性氧自由基(ROS)的积累所致,而这一积累过程需要铁离子的参与。多种物质和外界条件可引发铁死亡。小分子erastin通过抑制质膜上的胱氨
细胞有很多种死亡方式,包括凋亡、自噬和坏死。近年来,“铁死亡”(ferroptosis)作为一种新的细胞坏死方式逐渐进入了人们的眼帘。不同于通常的细胞坏死,铁死亡是一种受调控的坏死过程。
铁死亡是由于膜脂修复酶——谷胱甘肽过氧化物酶(GPX4)失效,造成膜脂上活性氧自由基(ROS)的积累所致,而这一积累过程需要铁离子的参与。多种物质和外界条件可引发铁死亡。小分子erastin通过抑制质膜上的胱氨酸-谷氨酸交换体,降低了细胞对胱氨酸的获取,使得GPX4的底物——谷胱甘肽合成受阻,进而引发膜脂ROS的积累和铁死亡。此外,另一种小分子RSL3作为GPX4的抑制剂也可引发铁死亡。当GPX4基因被敲除后,小鼠会因出现肾衰竭而死亡。
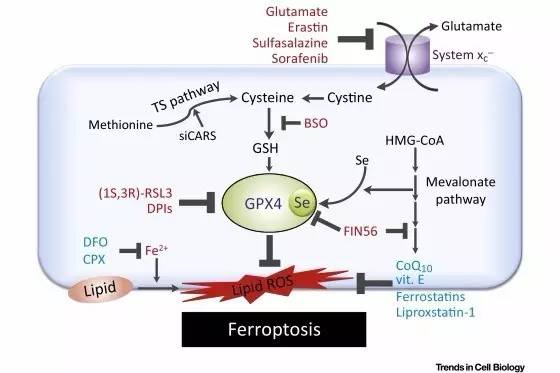
▲细胞铁死亡机制(图片来源:《Trends in Cell Biology》)
铁死亡与肿瘤抑制、神经元退化、抗病毒免疫反应和缺血-再灌注损伤等多种生理和病理过程有关。站在药物研发的角度,我们可以促进铁死亡,以清除有害的癌细胞、病毒感染的细胞等;或者抑制铁死亡,以保护健康细胞。当然,这一切可能的治疗思路都需建立在对铁死亡机理的理解上。
最近,德国亥姆霍兹慕尼黑中心(Helmholtz Zentrum München)的科学家们发现了铁死亡发生过程中的一个关键蛋白——ACSL4,并且找到了能够有效抑制铁死亡过程的小分子抑制剂。他们的成果发表在近期的《自然》子刊《Nature Chemical Biology》上。

▲本篇论文发表在了《自然》子刊上(图片来源:《Nature Chemical Biology》)
研究人员首先以小鼠胚胎成纤维细胞(MEF)为实验对象,发现当ACSL4基因被敲除后,上述细胞在RSL3的诱导下便不会再发生铁死亡。ACSL4是长链脂酰CoA合成酶(ACSL)家族的一员,在体内催化合成脂酰CoA,作为脂肪酸分解代谢的第一步反应。不同于ACSL4,在MEF中敲除ACSL家族的其他酶并不会引起铁死亡。
ACSL4在功能上有什么特别之处呢?原来,ACSL4将长链多不饱和脂肪酸活化,以参与膜磷脂的合成。其中,ACSL4能将花生四烯酸和肾上腺酸分别合成为花生四烯酰CoA和肾上腺酰CoA,以使其参与磷脂酰乙醇胺或磷脂酰肌醇等带负电膜磷脂的合成,成为其一部分。这些膜上的长链多不饱和脂肪酸常常可被氧化,特别是在RSL3等因素的诱导下,从而引发细胞的铁死亡。

▲花生四烯酸(左)和肾上腺酸(右)结构(图片来源:维基百科)
研究者指出,ACSL4就是通过参与合成这些易被氧化的膜磷脂而成为引发铁死亡的必需组分之一,使得细胞对RSL3等诱导因素敏感。ACSL4的这一角色不仅在MEF得到支持,而且在三阴性乳腺癌细胞系MDA-MB-157中得到进一步证实。这种乳腺癌细胞中有着较高水平的ACSL4,因此对RSL3十分敏感,而当ACSL4被敲除后,便不会因RSL3的诱导而发生铁死亡。
“这是一个十分有趣的结果,ACSL4可作为预测细胞是否可启动铁死亡程序的一个指标,” 文章的通讯作者José Pedro Friedmann Angeli博士说道。

▲文章通讯作者Marcus Conrad博士(左)和José Pedro Friedmann Angeli博士(右)(图片来源:亥姆霍兹慕尼黑中心官网)
因此,如果能抑制ACSL4,便可能保护细胞免受铁死亡。幸运的是,人们之前已发现了ACSL4的选择性抑制剂——噻唑烷二酮(thiazolidinedione)类物质,一类二型糖尿病药物。研究者发现,rosiglitazone、pioglitazone和troglitazone三种噻唑烷二酮类物质均能保护ACSL4基因被敲除的MEF细胞,使其在RSL3诱导下不会出现膜脂氧化和铁死亡,并且还能显著延长ACSL4基因敲除小鼠的生存期。其中,troglitazone的效果最明显。
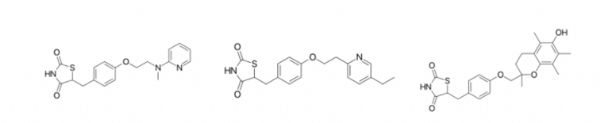
▲Rosiglitazone(左)、pioglitazone(中)和troglitazone(右)结构
(图片来源:维基百科)
“我们揭示了ACSL4酶在细胞死亡中的重要作用,这提示着一套全新的治疗思路,即可通过抑制细胞铁死亡用于神经退行性疾病的治疗,以及通过激发细胞铁死亡以用于某些癌症的治疗,”文章的另一位通讯作者Marcus Conrad博士表示:“某些用标准化疗难以对付的肿瘤可能适合于接受激发铁死亡的疗法。”
原始出处:
Doll S1, Proneth B1, Tyurina YY2, Panzilius E3, Kobayashi S1, Ingold I1, Irmler M4, Beckers J4, Aichler M5, Walch A5, Prokisch H6,7, Trümbach D1, Mao G2, Qu F2, Bayir H2, Füllekrug J8, Scheel CH3, Wurst W1, Schick JA1, Kagan VE2, Angeli JP1, Conrad M1.ACSL4 dictates ferroptosis sensitivity by shaping cellular lipid composition.Nat Chem Biol. 2016 Nov 14
Yang WS1, Stockwell BR2.Ferroptosis: Death by Lipid Peroxidation.Trends Cell Biol. 2016 Mar
Friedmann Angeli JP1, Schneider M2, Proneth B1, Tyurina YY3, Tyurin VA3, Hammond VJ4, Herbach N5, Aichler M6, Walch A6, Eggenhofer E7, Basavarajappa D8, Rådmark O8, Kobayashi S9, Seibt T1, Beck H10, Neff F6, Esposito I11, Wanke R5, Förster H1, Yefremova O1, Heinrichmeyer M1, Bornkamm GW12, Geissler EK7, Thomas SB13, Stockwell BR13, O'Donnell VB4, Kagan VE3, Schick JA1, Conrad M1.Inactivation of the ferroptosis regulator Gpx4 triggers acute renal failure in mice.Nat Cell Biol. 2014 Dec
Dixon SJ1, Stockwell BR2. The role of iron and reactive oxygen species in cell death.Nat Chem Biol. 2014 Jan
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Nat#
30
没有苏打水厉害
102
#癌细胞#
37
厉害了。
96
好新奇的方法啊
106