European Radiology:对于不同机构、不同机器、不同场强下进行的钆塞酸二钠增强MRI,是否仍可反应肝脏增强与肝功能的相关性?
2022-01-19 shaosai MedSci原创
钆塞酸二钠是一种肝细胞特异性对比剂,显示出选择性的肝细胞摄取,并在注射后约20分钟达到峰值(肝胆期)。
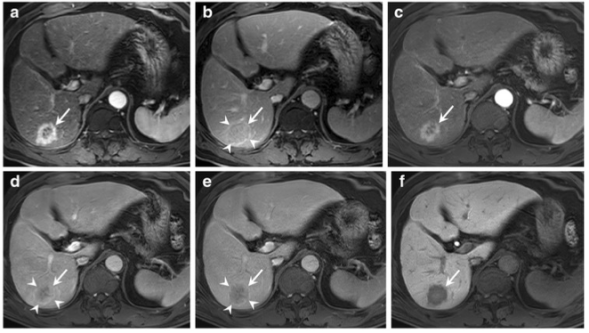
 钆塞酸二钠是一种肝细胞特异性对比剂,显示出选择性的肝细胞摄取,并在注射后约20分钟达到峰值(肝胆期)。肝胆期图像通过增强病变和健康肝脏组织之间的对比度差异来提高原发性和继发性肝脏肿瘤的检测率。与CT相比,钆塞酸二钠增强MRI可以改善基于肿瘤范围的治疗决策制定。以往的研究表明,肝脏强化与ALBI评分、Child-Pugh分级、MELD评分、低白蛋白血症、高胆红素血症、INR、血小板计数、血钠和腹水有关。然而,肝脏的信号强度受到多种因素的影响,包括扫描仪类型、场强和成像序列参数。Okada等专首次报道了使用肝脾比(LSR)对生化参数和肝胆相位增强之间的相关性进行的多中心研究,结果显示,在一个亚洲队列中,凝血酶活性、胆红素和总胆固醇水平与肝脏增强明显相关。然而,文献中缺乏对不同品牌扫描仪之间基于SI指数的一致性的评估。
钆塞酸二钠是一种肝细胞特异性对比剂,显示出选择性的肝细胞摄取,并在注射后约20分钟达到峰值(肝胆期)。肝胆期图像通过增强病变和健康肝脏组织之间的对比度差异来提高原发性和继发性肝脏肿瘤的检测率。与CT相比,钆塞酸二钠增强MRI可以改善基于肿瘤范围的治疗决策制定。以往的研究表明,肝脏强化与ALBI评分、Child-Pugh分级、MELD评分、低白蛋白血症、高胆红素血症、INR、血小板计数、血钠和腹水有关。然而,肝脏的信号强度受到多种因素的影响,包括扫描仪类型、场强和成像序列参数。Okada等专首次报道了使用肝脾比(LSR)对生化参数和肝胆相位增强之间的相关性进行的多中心研究,结果显示,在一个亚洲队列中,凝血酶活性、胆红素和总胆固醇水平与肝脏增强明显相关。然而,文献中缺乏对不同品牌扫描仪之间基于SI指数的一致性的评估。
近日,发表在European Radiology杂志的一项研究在一项前瞻性随机对照试验中收集的肝细胞肝癌(HCC)患者的多厂商研究队列中,钆塞酸二钠增强MRI是否仍存在肝脏增强和肝功能之间的关联性,为进一步的数据汇总及评估提供了参考依据。
本研究在一项前瞻性的多中心II期试验(SORAMIC)中,评估了359名使用不同扫描仪进行标准化钆塞酸二钠增强MRI扫描的患者图像。使用单变量和多变量分析,分析了肝胆期上的肝脏强化与生化实验室参数、肝功能相关的临床结果、肝功能分级系统(Child-Pugh和白蛋白-胆红素[ALBI])以及扫描仪特征之间的相关性。
LSR与白蛋白(rho = 0.193;p < 0.001)、血小板计数(rho = 0.148;p = 0.004)和钠(rho = 0.161;p = 0.002)之间存在明显的正相关;LSR与总胆红素(rho = -0.215;p < 0.001)和AST(rho = -0.191;p < 0.001)之间存在负相关性。多变量分析证实了白蛋白(p = 0.022)、总胆红素(p = 0.045)、AST(p = 0.031)、血小板计数(p = 0.012)和钠(p = 0.006)各自的独立意义。腹水(1.47 vs. 1.69,p < 0.001)和静脉曲张(1.55 vs. 1.69,p = 0.006)的存在与LSR明显降低有关。同样,ALBI 1级患者的LSR明显高于2级患者(1.74 ± 0.447 vs. 1.56 ± 0.408,p < 0.001);Child-Pugh A患者的LSR明显高于Child-Pugh B(1.67 ± 0.44 vs. 1.49 ± 0.33,p = 0.021)。另外,LSR与MELD-Na评分呈负相关(rho = -0.137; p = 0.013)。然而,一个扫描仪品牌与较低的LSR明显相关(p < 0.001)。
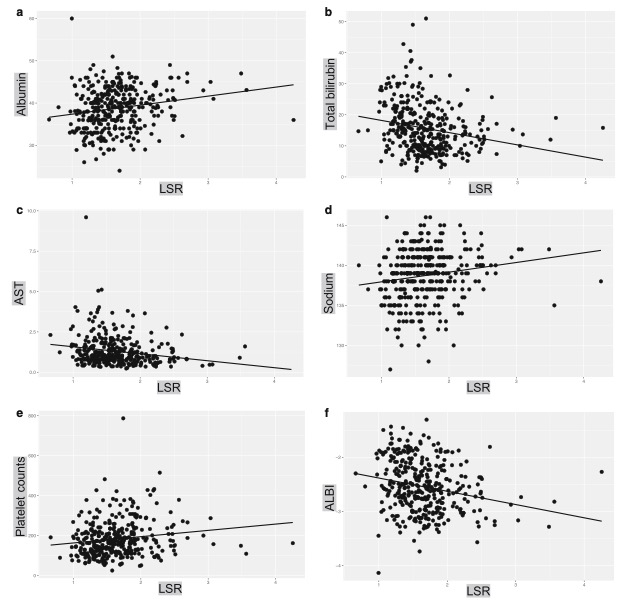
图 LSR与生化参数之间的相关性。线性回归线的散点图显示LSR与具有统计学意义的变量的关系:(a)白蛋白(rho = 0.193,p < 0.001),(b)总胆红素(rho = -0.215,p < 0.001),(c)AST (rho =−0.191, p < 0.001),(d)钠(rho = 0.161, p = 0.002), (e) 血小板计数(rho = 0.148, p = 0.004), 和(f) ALBI评分(rho = -0.225, p < 0.001)。ALBI,白蛋白-胆红素;AST,天门冬氨酸转氨酶;LSR,肝脏与脾脏比率。
本研究表明,在几个中心和场强之间,无论是否有潜在的肝硬化,HCC患者在钆塞酸二钠增强MRI的肝胆期上的增强与肝功能均存在相关性。这强调了钆塞酸二钠增强MRI作为肝功能的影像学标志物在治疗决策过程中的重要性,为患者肝功能的一致性评估及肝特异性对比剂更广泛的应用提供了数据支持。
原文出处:
Osman Öcal,Bora Peynircioglu,Christian Loewe.Correlation of liver enhancement in gadoxetic acid-enhanced MRI with liver functions: a multicenter-multivendor analysis of hepatocellular carcinoma patients from SORAMIC trial.DOI:10.1007/s00330-021-08218-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#钆塞酸二钠#
71
#相关性#
42
#PE#
64
#肝功能#
40
#机器#
74