Neurology:脑淀粉样血管病患者CSF生物标志物概况分析!
2018-02-01 xing.T MedSci原创
由此可见,Aβ42、Aβ40、t-tau和p-tau的特异性CSF模式可能是CAA的分子生物标志物,但需要在更大的CAA队列中进行分析。
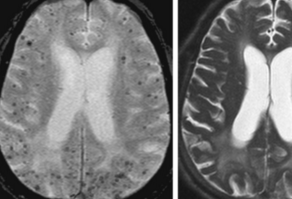
近日,神经病学领域权威取杂志Neurology上发表了一篇荟萃分析文章,该分析旨在评估4种核心CSF生物标志物(β-淀粉样蛋白[Aβ] 42、Aβ40、总tau[t-tau]和磷酸化tau[p-tau])哪些标志物在散发性脑中淀粉样血管病(CAA)中变化最大。
研究人员系统地检索了PubMed,查找报告了有症状散发性CAA队列与对照者和阿尔茨海默病患者反映淀粉样蛋白前体蛋白质代谢(Aβ42和Aβ40)、神经变性(t-tau)和缠结病理学(p-tau)疾病(AD)CSF生物标志物的研究。在基于生物标志物浓度平均比值(RoM)的随机效应荟萃分析来评估生物标志物的性能:(1)CAA的患者与健康对照者和(2)CAA患者与AD患者。 RoM>1表示CAA患者与对照人群相比生物标志物浓度较高,而RoM<1表示对照人群具有较高的浓度。
三项研究符合纳入标准。这些研究包含了5个CAA患者队列(n=59名患者)与健康对照者(n=94名参与者)和AD患者队列(n=158名患者)。CAA患者与对照者相比有三种核心生物标记物有所差异:CSF中Aβ42(RoM为0.49,95%可信区间[CI]为0.38-0.64,P<0.003)、Aβ40(RoM为0.70,95%CI为0.63-0.78,P<0.0001)以及t-tau(RoM为1.54,95%CI为1.15-2.07,P=0.004); p-tau则无差异(RoM为1.24,95%CI为0.99-1.54,P=0.062)。CAA患者和AD患者CSF中Aβ40的差异最大(RoM为0.76,95%CI为0.69-0.83,P<0.0001),但Aβ42无差异(RoM为1.00; 95%CI为0.81-1.23,P=0.970)。对于t-tau和p-tau,CAA患者与AD患者的平均CSF比值分别为0.63(95%CI为0.54-0.74,P<0.0001)和0.60(95%CI为0.50-0.71,P<0.0001) 。
由此可见,Aβ42、Aβ40、t-tau和p-tau的特异性CSF模式可能是CAA的分子生物标志物,但需要在更大的CAA队列中进行分析。
原始出处:
Andreas Charidimou,et al.Core CSF biomarker profile in cerebral amyloid angiopathy A meta-analysis.Neurology.2018.https://doi.org/10.1212/WNL.0000000000005030
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#脑淀粉样#
37
#血管病#
34
#CSF#
34
#Neurol#
0
#标志物#
31
#生物标志#
34
#生物标志#
21
#脑淀粉样血管病#
29
学习了新知识
92
学习了.涨知识
96