IBD: 使用过大麻的IBD患者住院时需要阿片类制剂的比例明显较高
2021-03-28 MedSci原创 MedSci原创
炎症性肠病(IBD)是一种慢性炎症性疾病,它的发病会对患者的生活质量产生一定影响,而且对于常规药物治疗的反应不一。
炎症性肠病(IBD)是一种慢性炎症性疾病,它的发病会对患者的生活质量产生一定影响,而且对于常规药物治疗的反应不一。阿片类镇痛药通常用于治疗IBD相关的疼痛,但是阿片类药物的使用会增加死亡率和感染的风险,最近的数据表明减少住院患者的阿片类药物暴露时间与降低住院时间(LOS)和较低的再入院率相关。目前尚不清楚的是,在IBD患者中通常用于缓解症状的入院前使用大麻是否会在患者无法使用大麻进行症状处理时增加住院患者阿片类药物暴露的风险。因此,本项研究旨在试图评估IBD患者入院前的大麻使用与住院后阿片类药物暴露之间的关联。

研究人员对2017年3月1日至2018年4月10日间因IBD住院的成年患者进行了一项回顾性队列研究。阿片类药物的暴露量的计算方式是通过将阿片类药物的剂量总和换算成静脉内吗啡毫克当量并除以停留时间得到的。使用多变量线性回归来评估大麻使用与住院患者阿片类药物暴露之间的关联,同时调整包括IBD严重性和入院前阿片类药物使用在内的混杂因素。
本项研究共包括423名IBD患者。线性回归分析显示,住院患者的阿片类药物暴露(静脉内吗啡毫克当量除以住院时间)与入院前使用大麻之间具有显着正相关(r= 12.1; 95%[CI],2.6-21.5)。其他显着相关的变量是患者首次报告的疼痛评分(r= 1.3; 95%CI,0.6-2.0)和入院前使用阿片类药物(r= 22.3; 95%CI,17.0-27.6)。
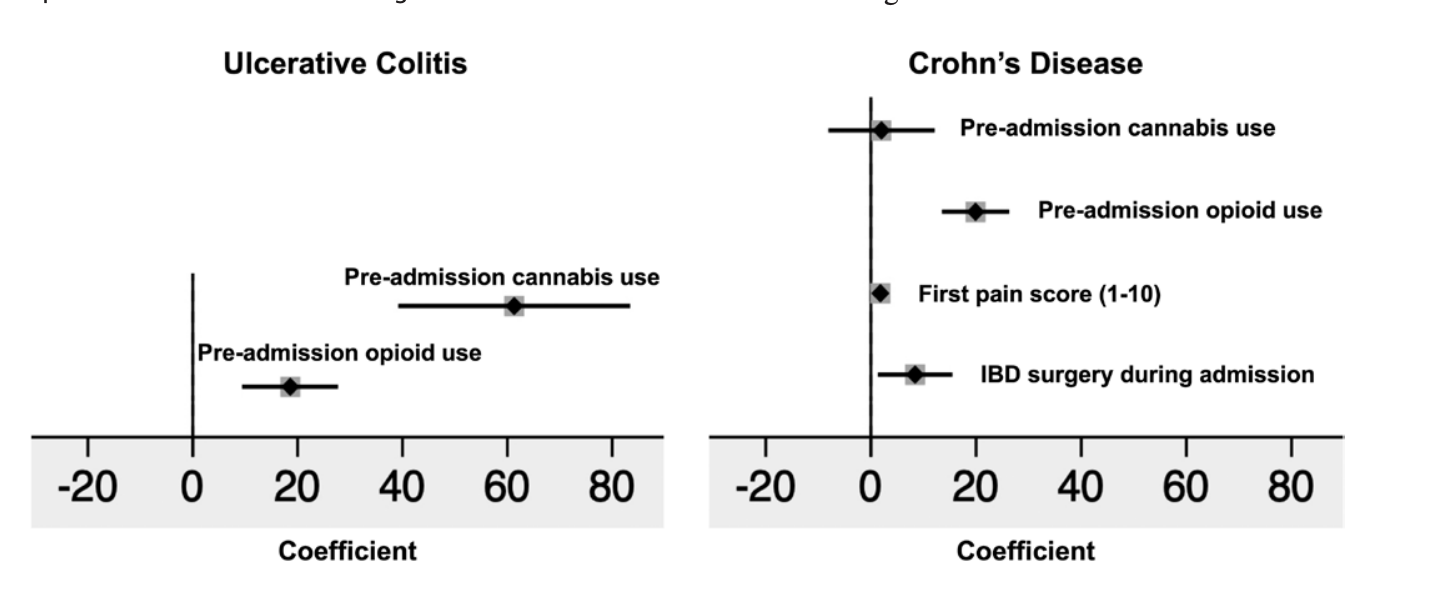
本项研究证实控制混杂因素后,大麻的使用与住院患者的阿片类药物暴露呈正相关。
原始出处:
Rahul S Dalal. Et al. Preadmission Cannabis Use Is Positively Correlated With Inpatient Opioid Dose Exposure in Hospitalized Patients With Inflammatory Bowel Diseases.Inflammatory Bowel Diseases.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#IBD#
38
#大麻#
36
#阿片类#
32
学到了很多东西谢谢老师
82