肝癌椎管内硬脊膜外转移1例
2020-02-12 缪逸涛 杨军 陈庚 中国临床神经外科杂志
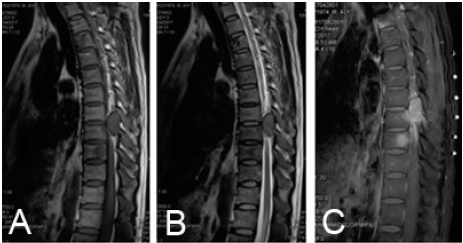
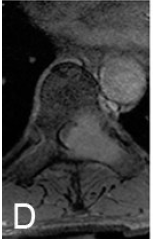
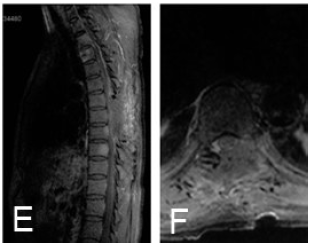
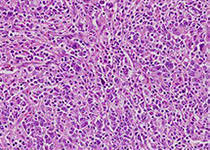
男,43岁,因胸背部持续性刺痛2个月加重10 d,伴双下肢无力、麻木逐渐加重、大小便功能障碍5 d入院。既往肺结核病史20年,乙型病毒性肝炎病史10年。入院前10 d当地县医院肺部CT检查示双肺上叶、右肺下叶陈旧性结核;胸8椎体水平椎管内异常稍高密度影。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










已读
95
#椎管内#
32
#椎管#
50
感觉这个术前没查清楚
83
#硬脊膜#
30
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
42