Eur J Cancer:肿瘤浸润淋巴细胞密度与免疫治疗的NSCLC患者预后正相关!
2021-02-01 MedSci原创 MedSci原创
免疫检查点抑制剂(ICI)是癌症治疗最重要的里程碑之一。对于非小细胞肺癌(NSCLC),ICI单药或与化疗或其他ICI联合使用均可较单用化疗提高患者存活率,现已成为NSCLC的标准治疗方案。
免疫检查点抑制剂(ICI)是癌症治疗最重要的里程碑之一。对于非小细胞肺癌(NSCLC),ICI单药或与化疗或其他ICI联合使用均可较单用化疗提高患者存活率,现已成为NSCLC的标准治疗方案。
肿瘤浸润性淋巴细胞(TIL)的形态评价与晚期NSCLC患者采用ICI或化疗的预后的相关性尚不明确。本研究是一项多中心回顾性研究,旨在分析TIL与晚期NSCLC患者采用ICI或化疗的预后的相关性。
该研究包括两个队列:纳武单抗队列:2012年11月-2017年2月期间采用纳武单抗治疗的221名患者;化疗队列:2009年6月-2016年10月期间接受化疗的189名患者。对具有可用于间质TIL评估的组织的患者进行分析。高TIL计数(高TIL)定义为≥10%密度。主要终点为总生存期(OS)。
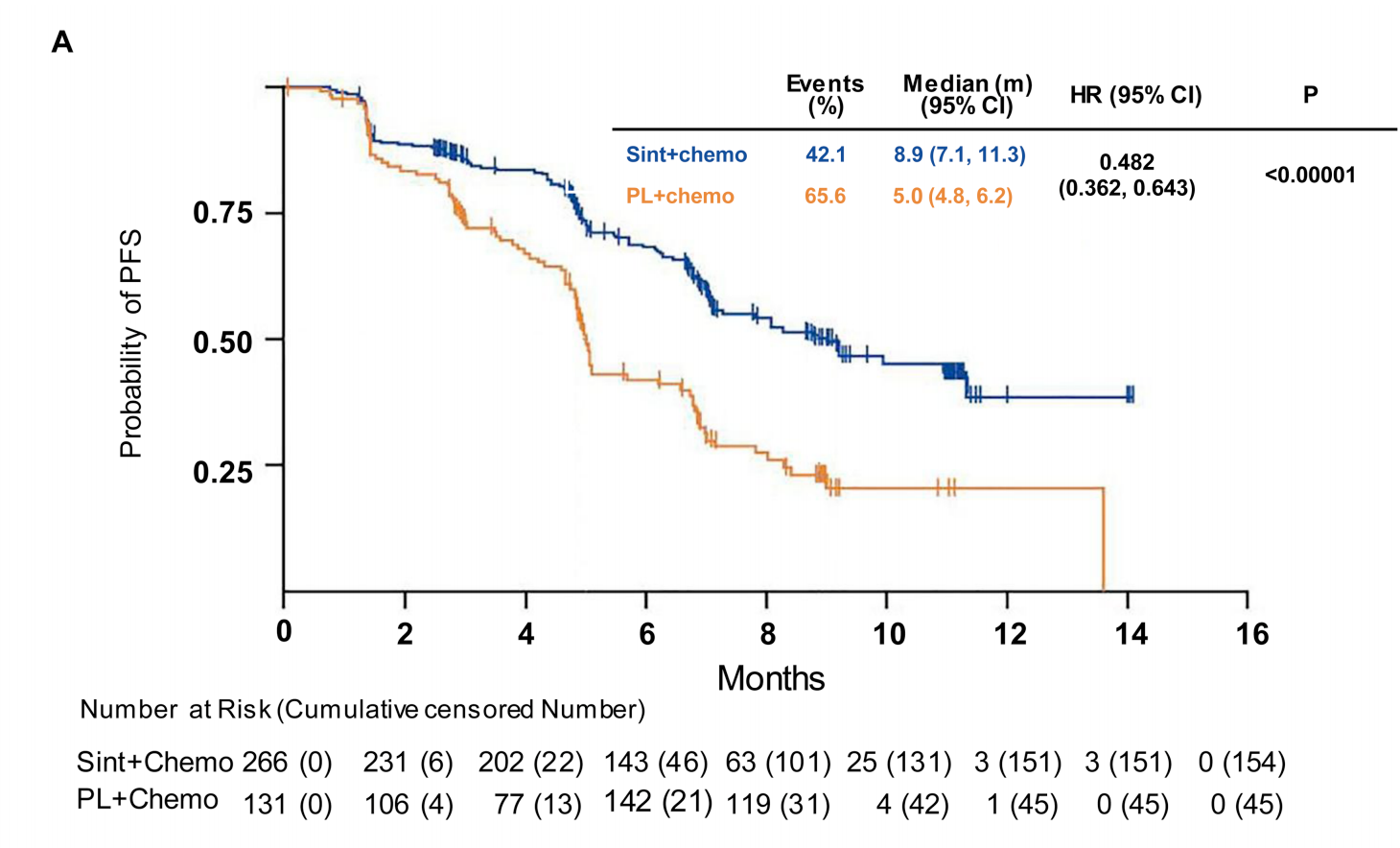
在纳武单抗队列中,64%为男性,中位年龄63岁,82.3%为吸烟者,77%的表现状态≤1分,63%为腺癌。高TIL发生率为22%,与OS和无进展生存率(PFS)相关(危险比[HR] 0.48,95%CI 0.28-0.81; 0.40, 95%CI 0.25-0.64)。高TIL组和低TIL组的中位PFS分别为13.0个月(95%CI 5.0-未达)和2.2个月(1.7-3.0),中位OS分别为未达到(12.2-未达到)和8.4个月(5.0-11.6)。高TIL与总有效率(ORR)和疾病控制率(DCR)相关(P均<0.0001)。
在化疗队列中,69%为男性,89%为吸烟者,86%的表现状态≤1分,90%为腺癌。高TIL发生率为37%。中位PFS和OS分别为5.7个月(95%CI 4.9-6.7)和11.7个月(9.3-13.0),均与TIL无关。
综上所述,在NSCLC患者的真实免疫治疗队列中,高TIL与良好的预后相关,但与采用化疗的患者预后无关,提示TIL或可用于筛选适合免疫治疗的患者。
原始出处:
Gataa Ithar,Mezquita Laura,Rossoni Caroline et al. Tumour-infiltrating lymphocyte density is associated with favourable outcome in patients with advanced non-small cell lung cancer treated with immunotherapy. Eur J Cancer, 2021, 145: 221-229.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#患者预后#
32
#正相关#
33
#SCLC患者#
30
在NSCLC患者的真实免疫治疗队列中,高TIL与良好的预后相关
78
#淋巴细胞#
40
#NSCLC患者#
27
NSCLC下一步突破在于新靶点了,靶向治疗和免疫治疗基本见顶了,再有新的就需要新机制了
66
学习了
104
认真学习了。
73