J Clin Oncol:长春新碱-伊立替康方案加用替莫唑胺可改善复发/难治性横纹肌肉瘤患者的生存预后
2021-09-16 Nebula MedSci原创
长春新碱-伊立替康方案加用替莫唑胺可改善复发/难治性横纹肌肉瘤患者的生存预后
横纹肌肉瘤(RMS)一旦复发,往往就对现有治疗不敏感了,导致总存活率不足 20%。复发后的主要预后因素是复发类型、既往放疗、初始肿瘤大小和确诊后复发的时间。当下迫切需要新的系统疗法来改善复发性 RMS 患者的预后。
VIT-0910 试验旨在评估长春新碱-伊立替康联合或不联合替莫唑胺(VIT 或 VI)治疗复发性或难治性横纹肌肉瘤的疗效和安全性。
这是一项随机 2 期试验,0.5-50 岁的 RMS 患者接受了 21 天为一疗程的 长春新碱+伊立替康±替莫唑胺治疗,直到病情进展或出现不可耐受的毒性。主要终点是两个疗程后的客观缓解率。次要终点包括最佳缓解情况。无进展生存期、总生存期和不良反应。
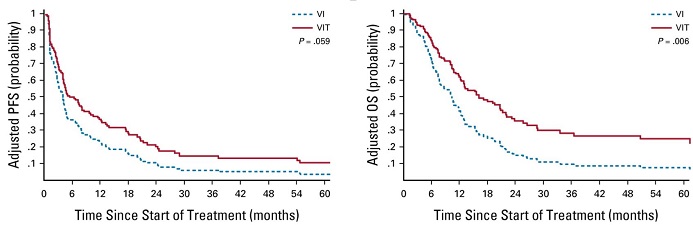
两治疗组的校正PFS和OS
从 37 个医疗中心共招募了 120 位患者(每组 60 位)。受试患者的中位年龄为 11 岁(范围 0.5-45 岁),89% 的患者为复发性 RMS。VIT 组和 VI 组的客观缓解率分别是 44% vs 31%(校正优势比 0.50, 95% CI 0.22-1.12, P=0.09)。VIT 组的总生存期显著优于 VI 组(校正风险比 0.55, 95% CI 0.35-0.84, P=0.006),无进展生存期亦是如此(0.68, 95% CI 0.46-1.01, P=0.059)。
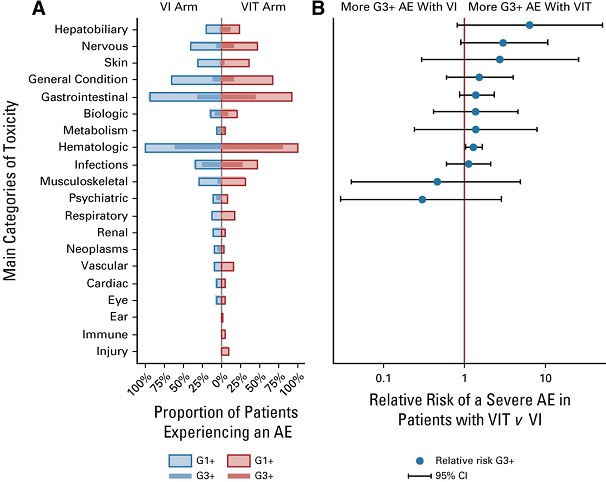
两组的毒性反应和相对风险比
总体上,VIT 组患者经历的 3 级及以上的不良反应事件多于 VI 组(98% vs 78%;P=0.009),包括血液学毒性反应也存在明显差异(81% vs 61%;P=0.025)。
综上,在 VI 方案中加用替莫唑胺可提高复发性横纹肌肉瘤的化疗效果,但伴随的毒性反应也增多。VIT 方案被认为是欧洲儿科软组织肉瘤患者的新标准治疗方法。
原始出处:
Anne-Sophie Defachelles, et al. Randomized Phase II Trial of Vincristine-Irinotecan With or Without Temozolomide, in Children and Adults With Relapsed or Refractory Rhabdomyosarcoma: A European Paediatric Soft Tissue Sarcoma Study Group and Innovative Therapies for Children With Cancer Trial. Journal of Clinical Oncology. https://ascopubs.org/doi/10.1200/JCO.21.00124
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#生存预后#
47
#长春新碱#
50
#Oncol#
38
#难治性#
37
厉害了!
63
谢谢梅斯分享这么多精彩信息
65