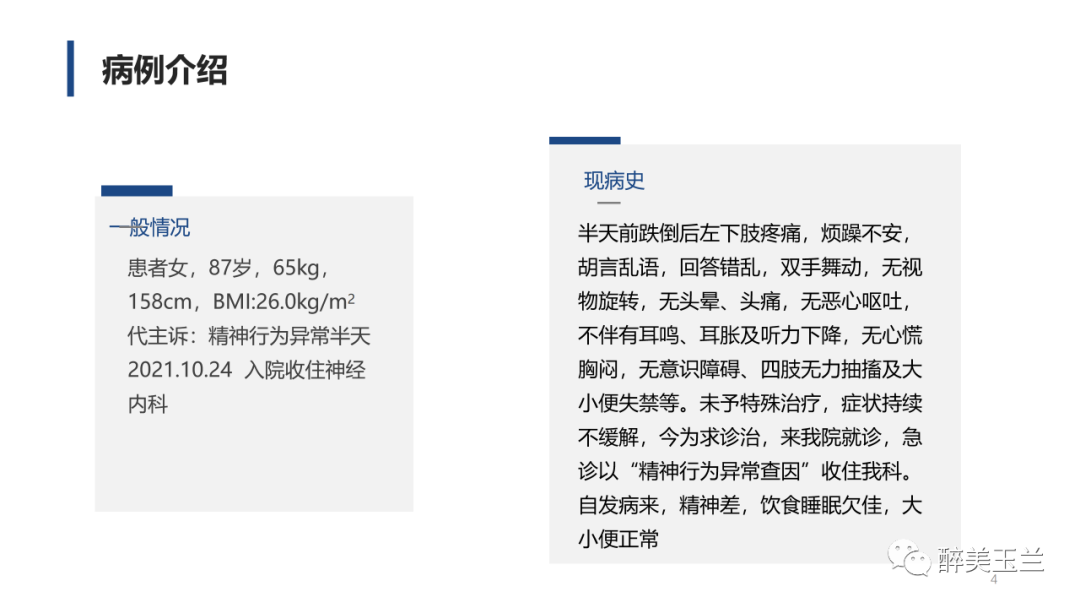
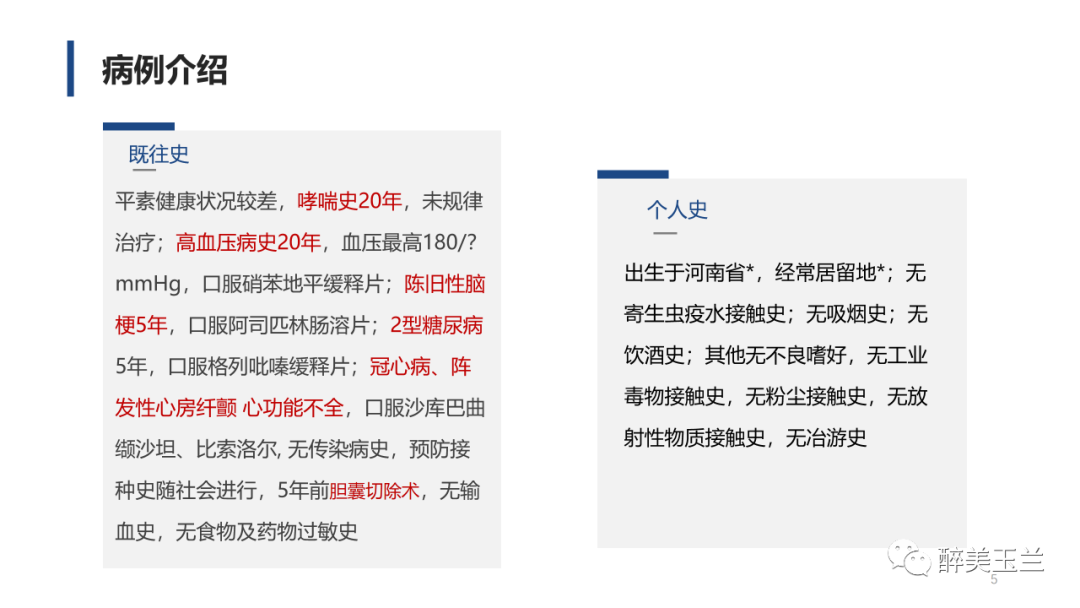
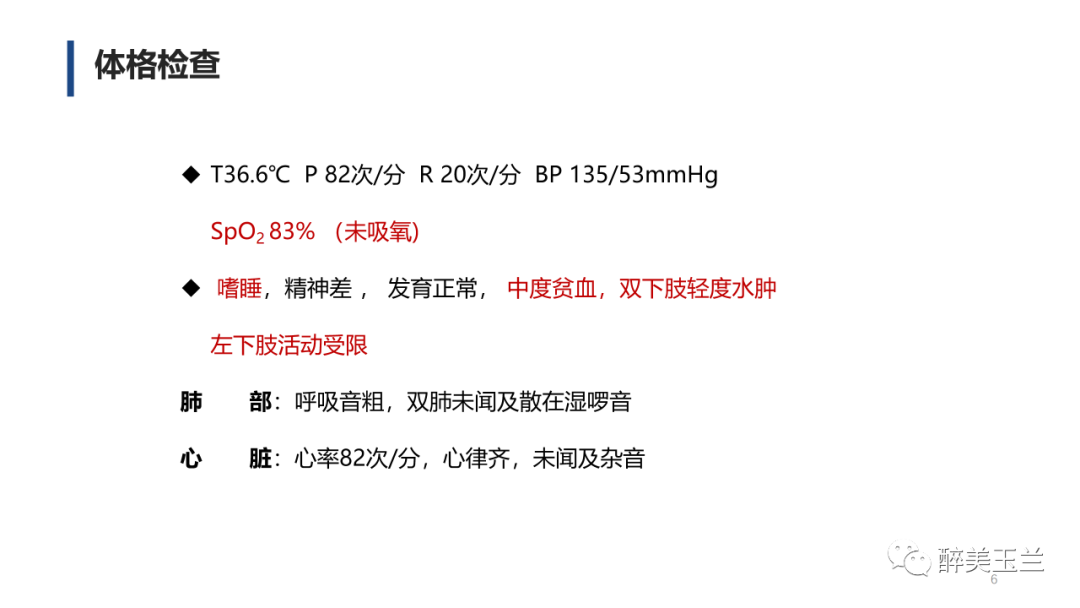
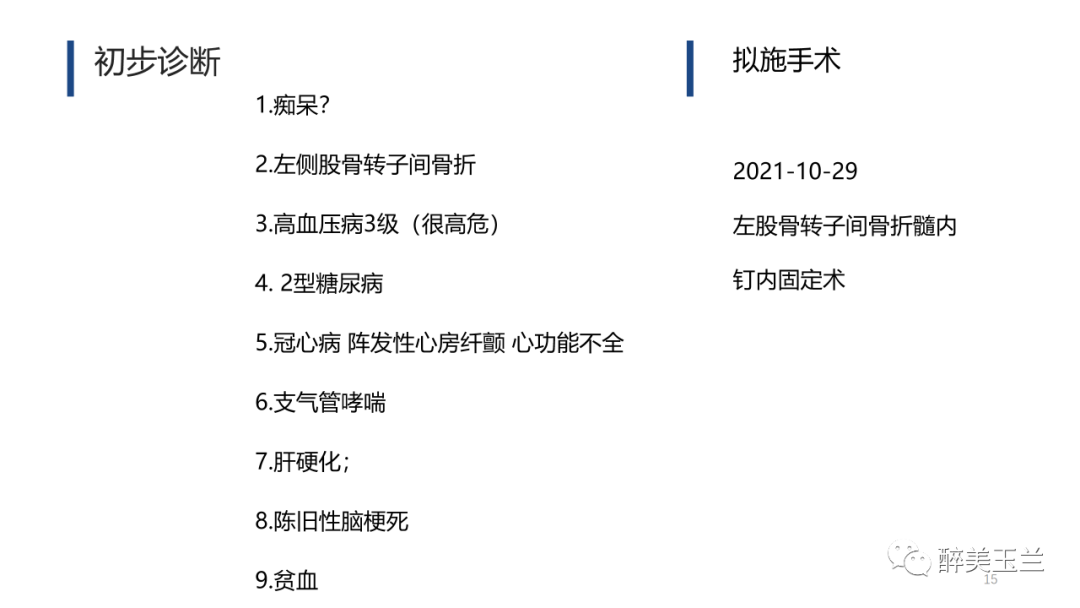
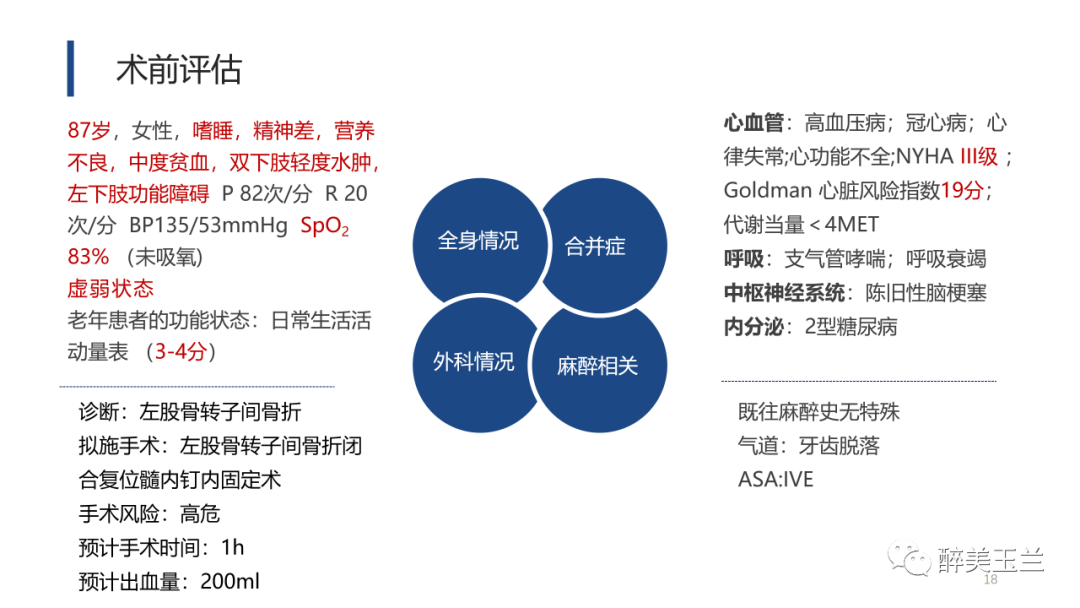
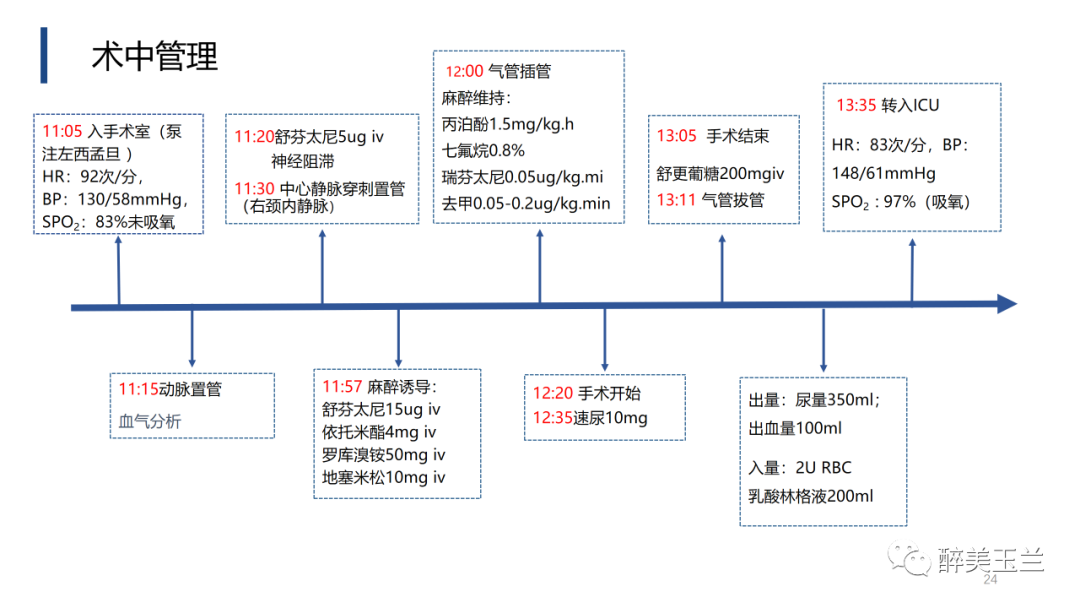
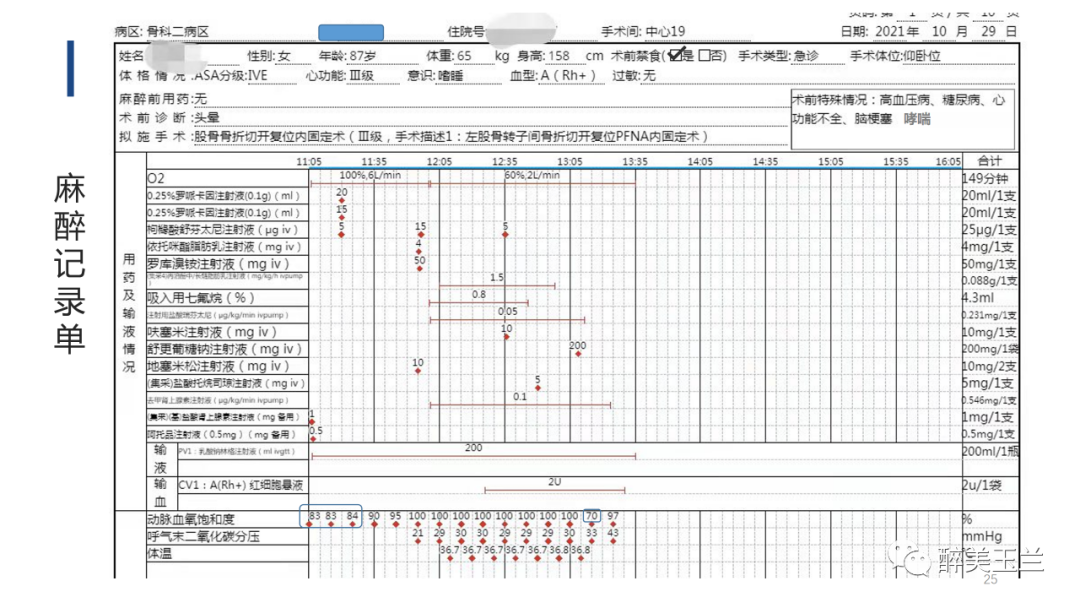
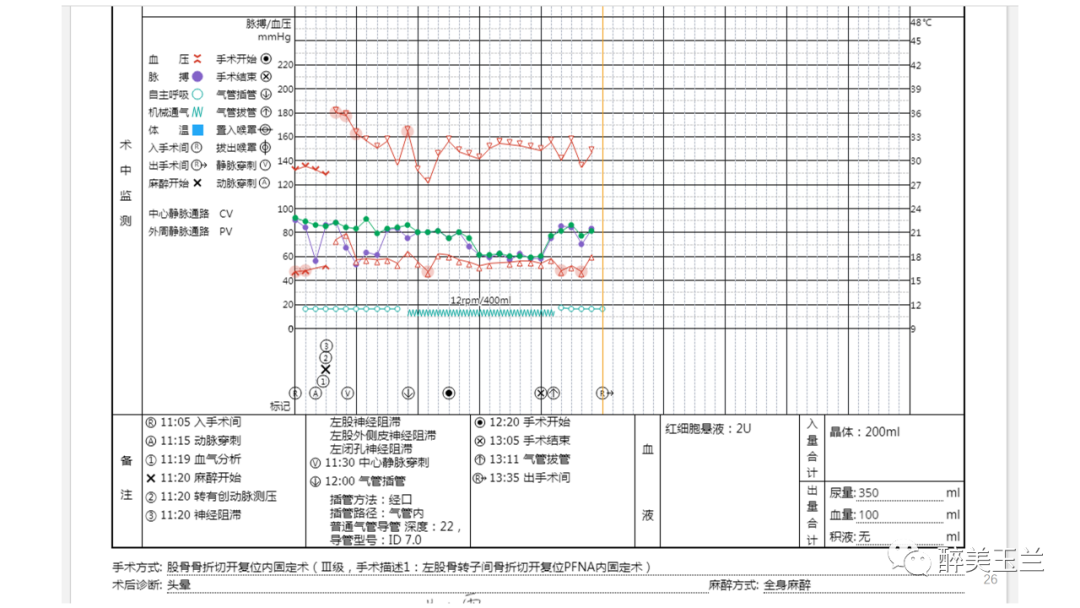
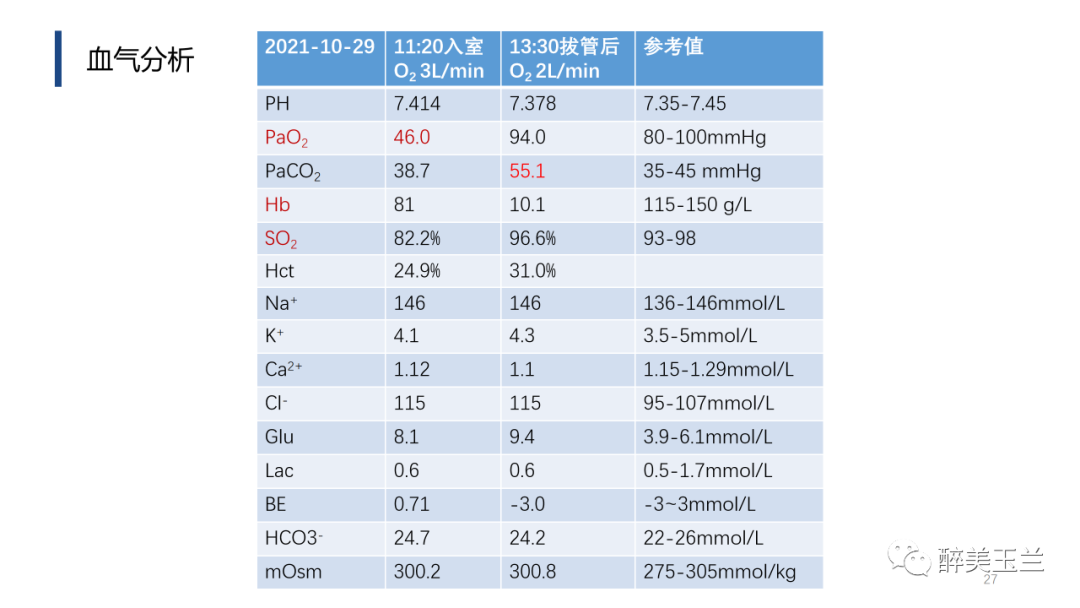
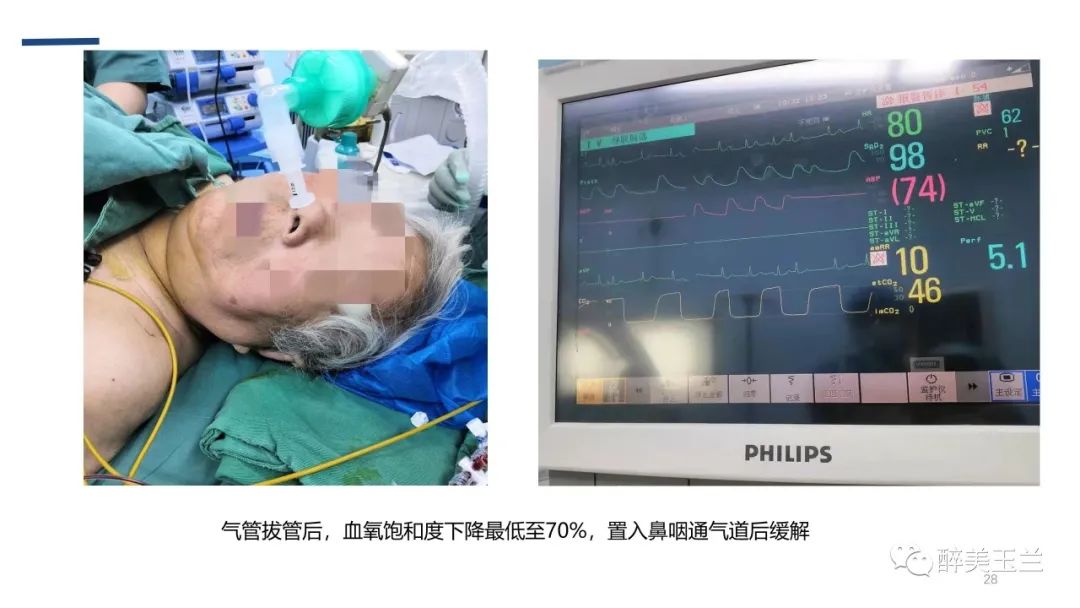
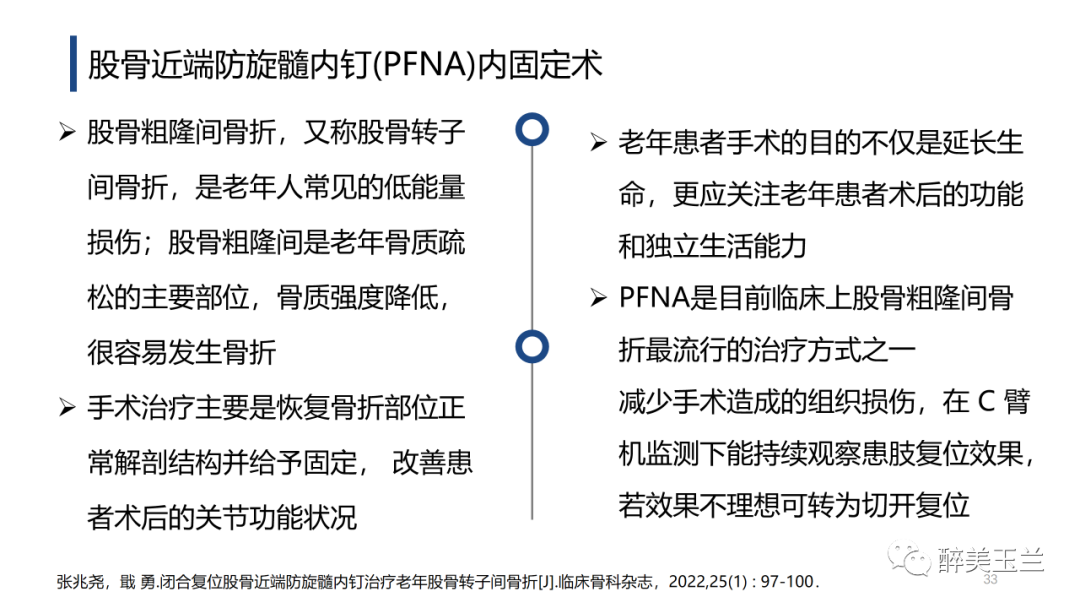
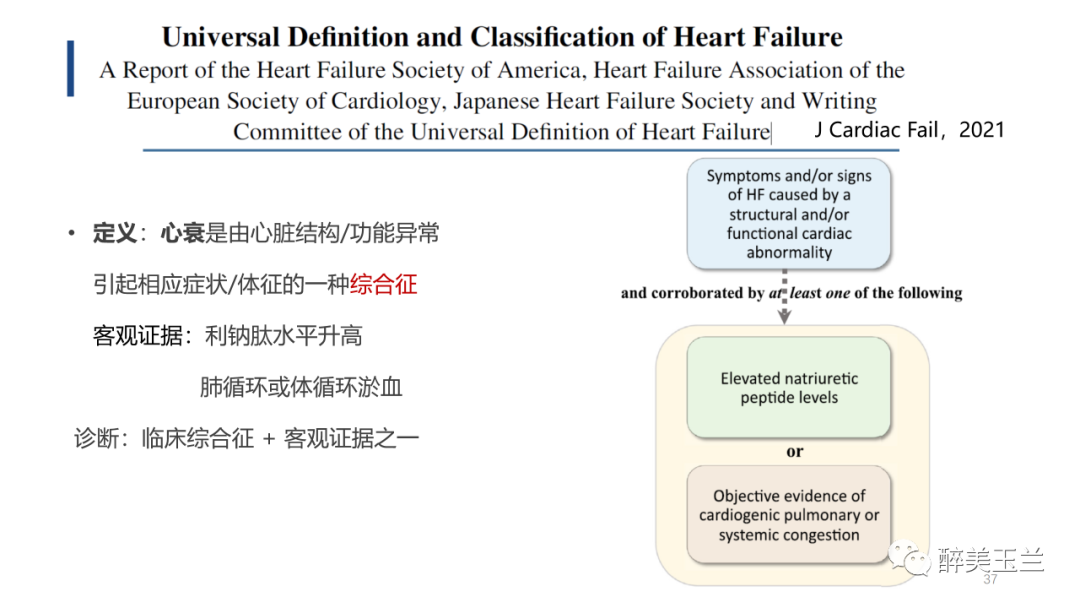
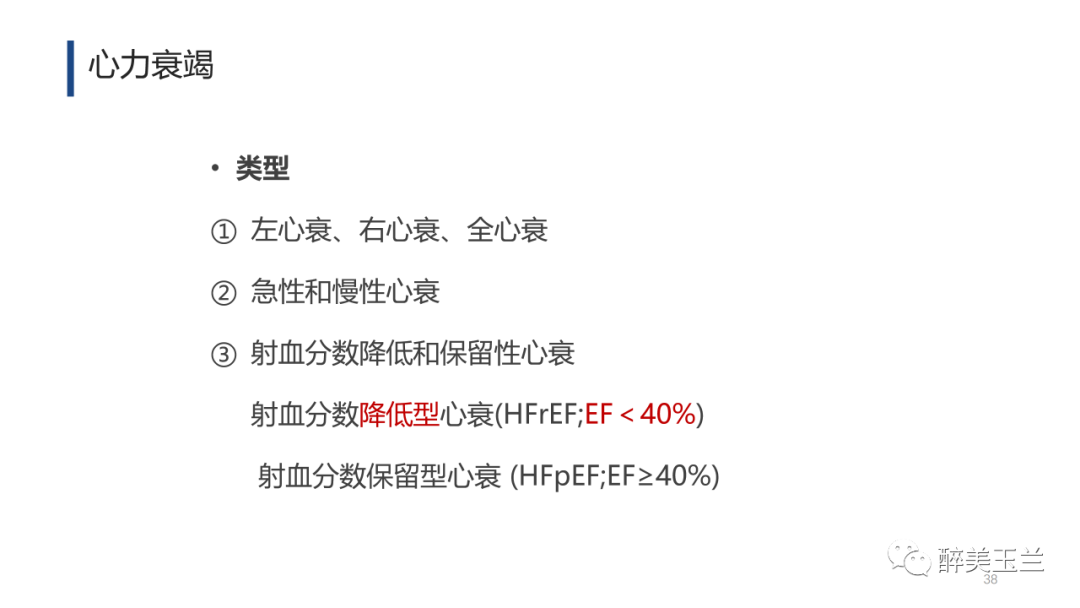
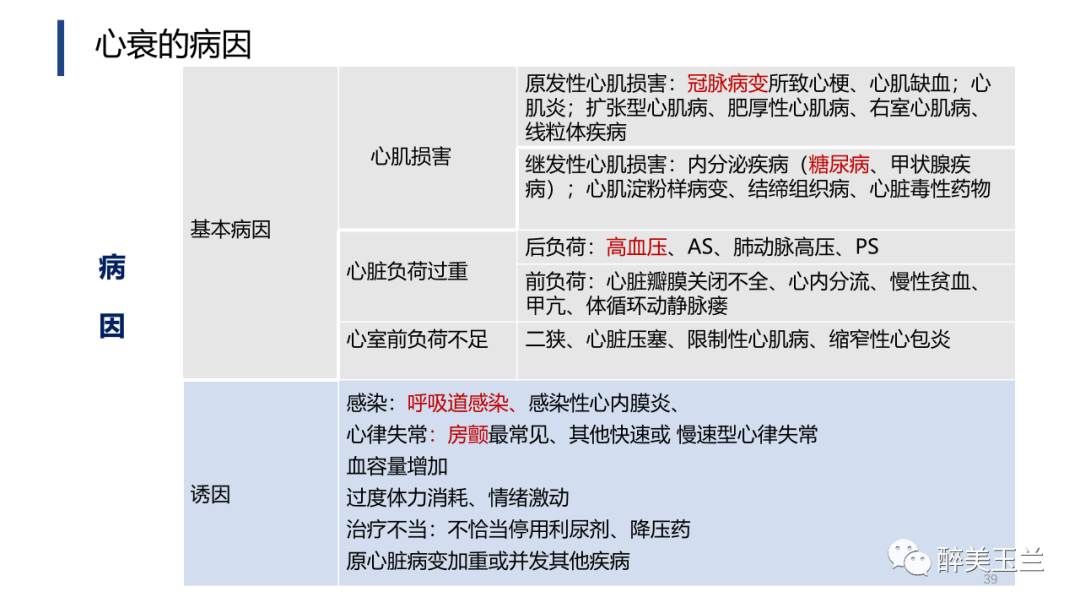
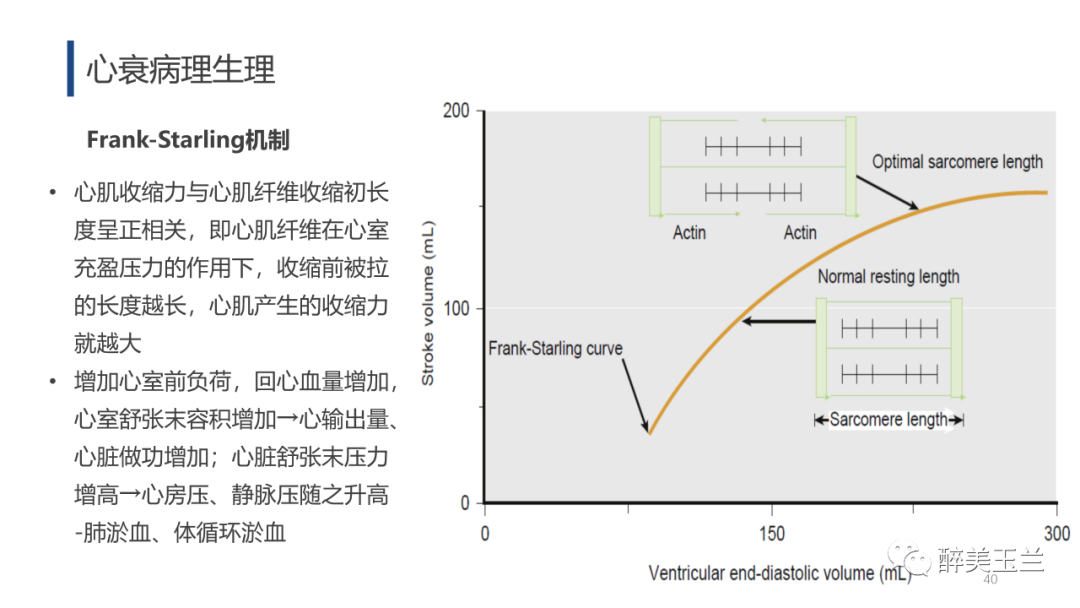
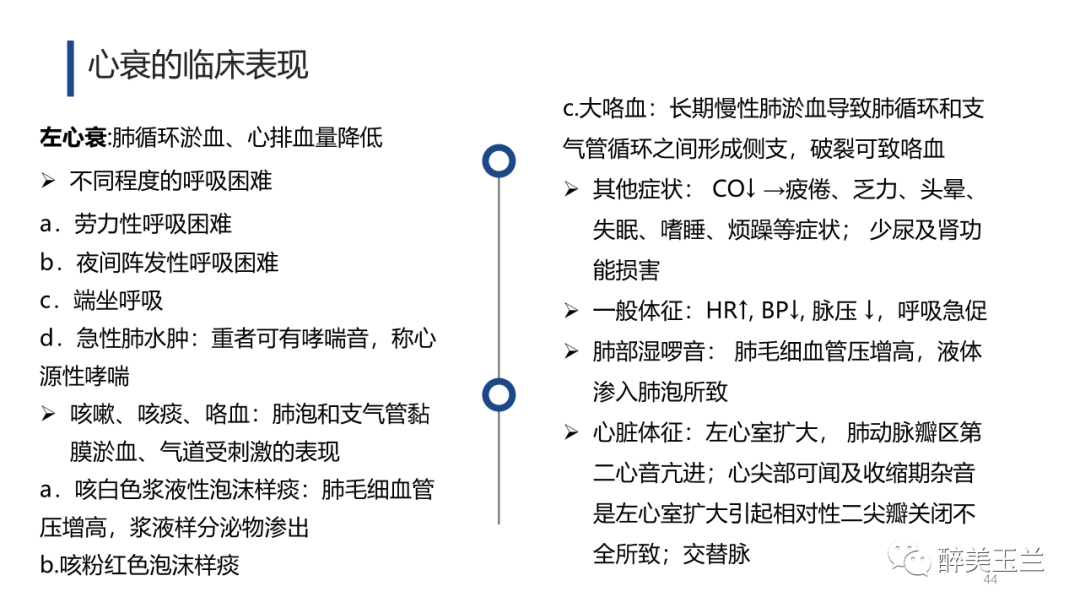
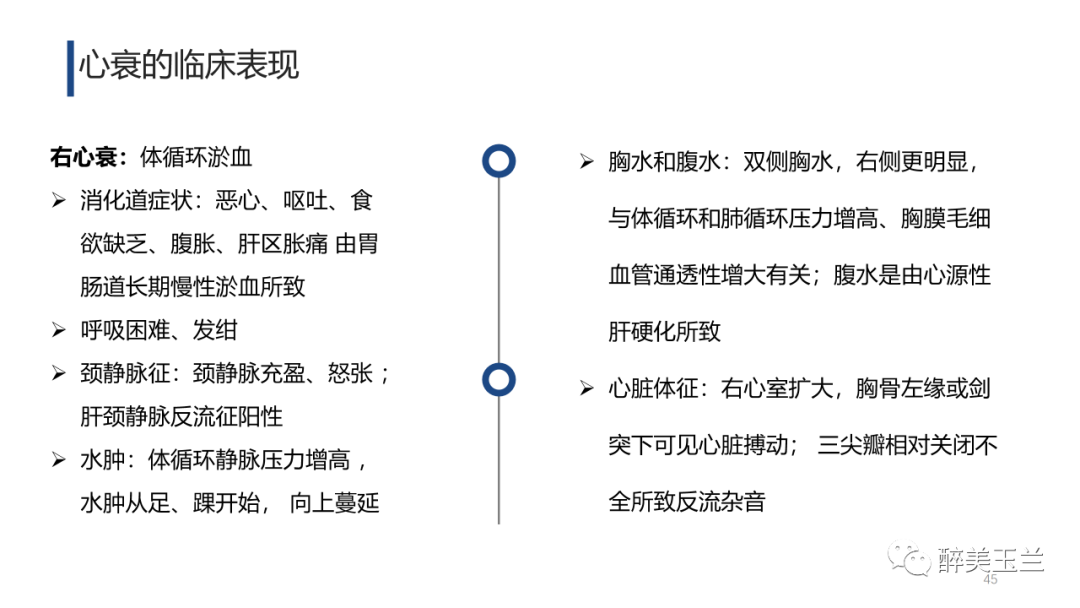
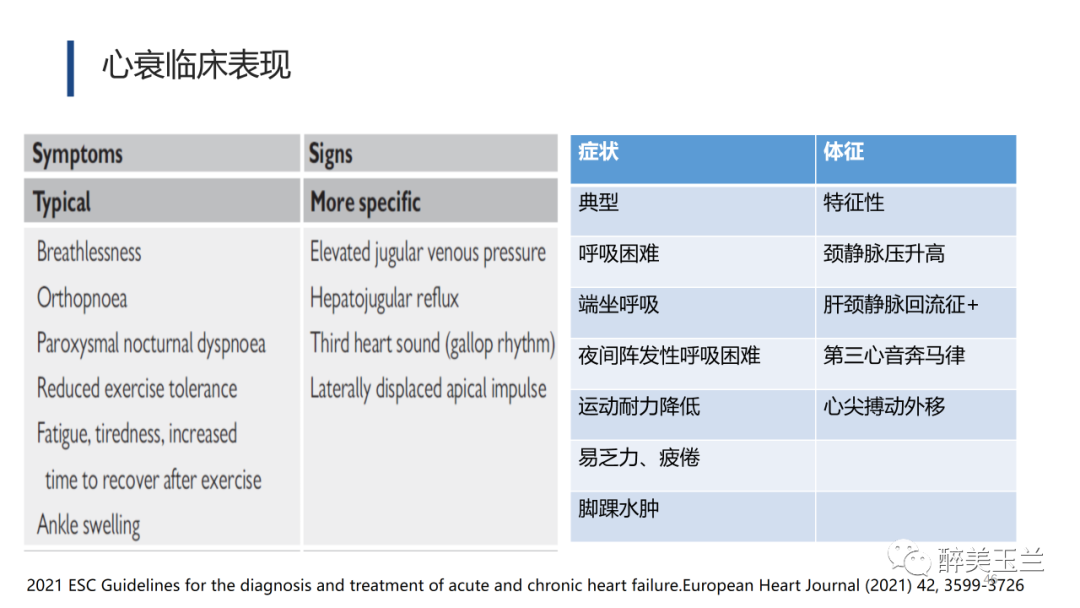
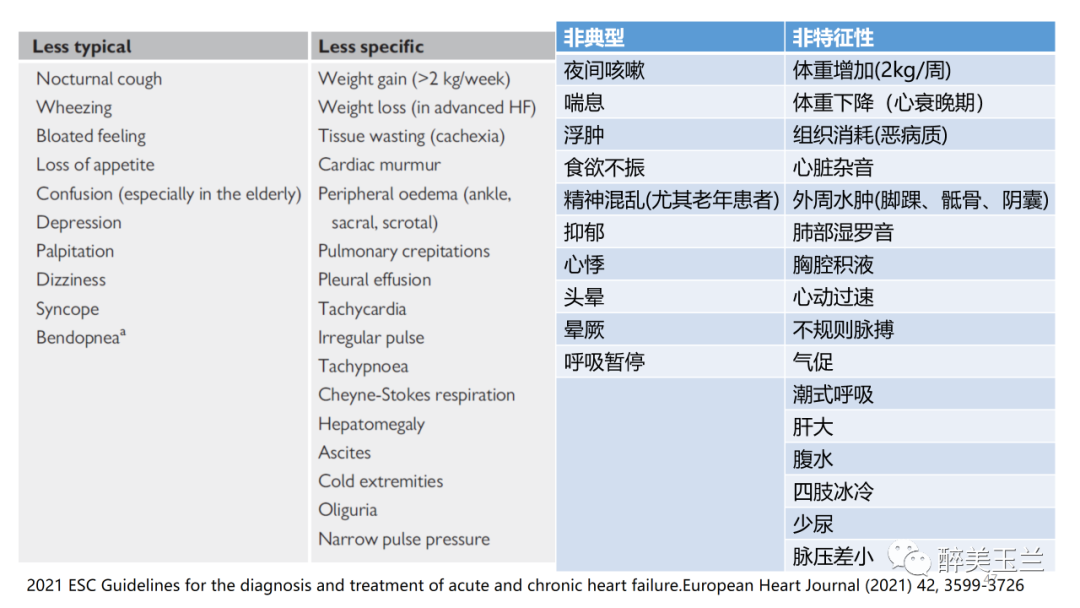
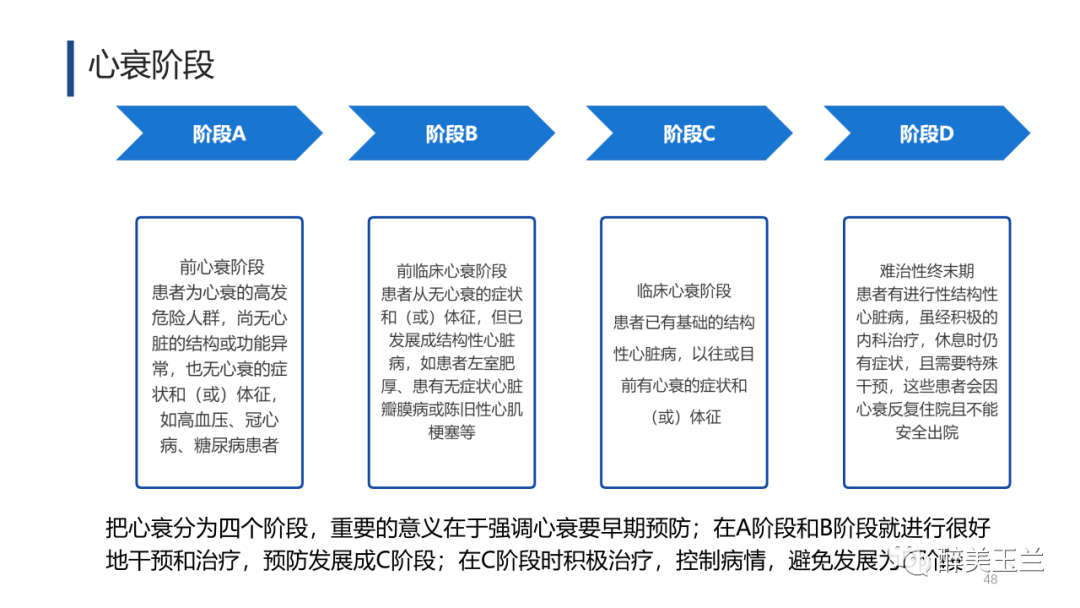
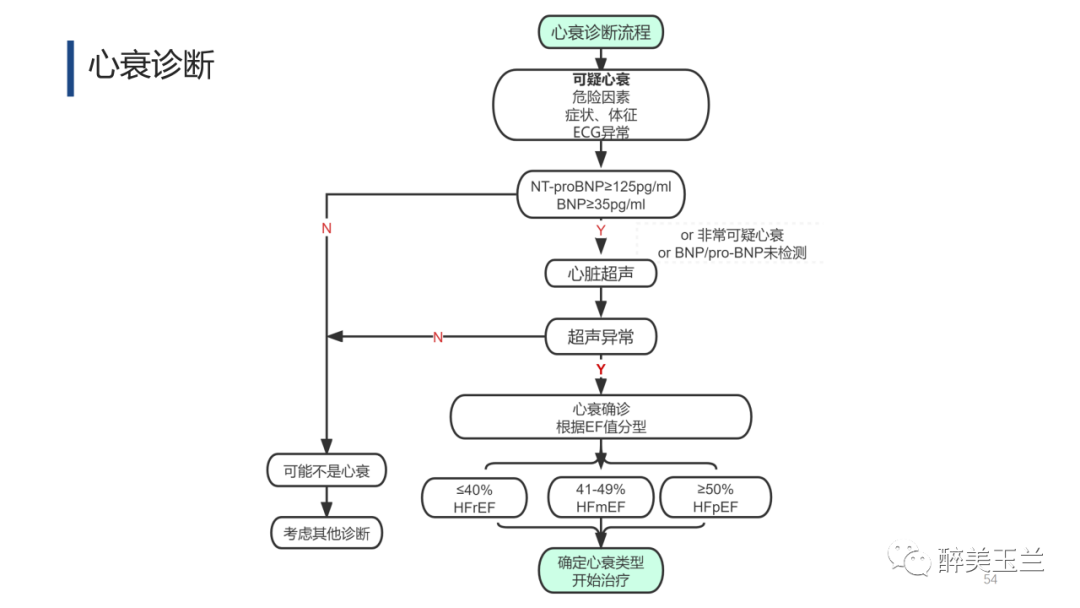
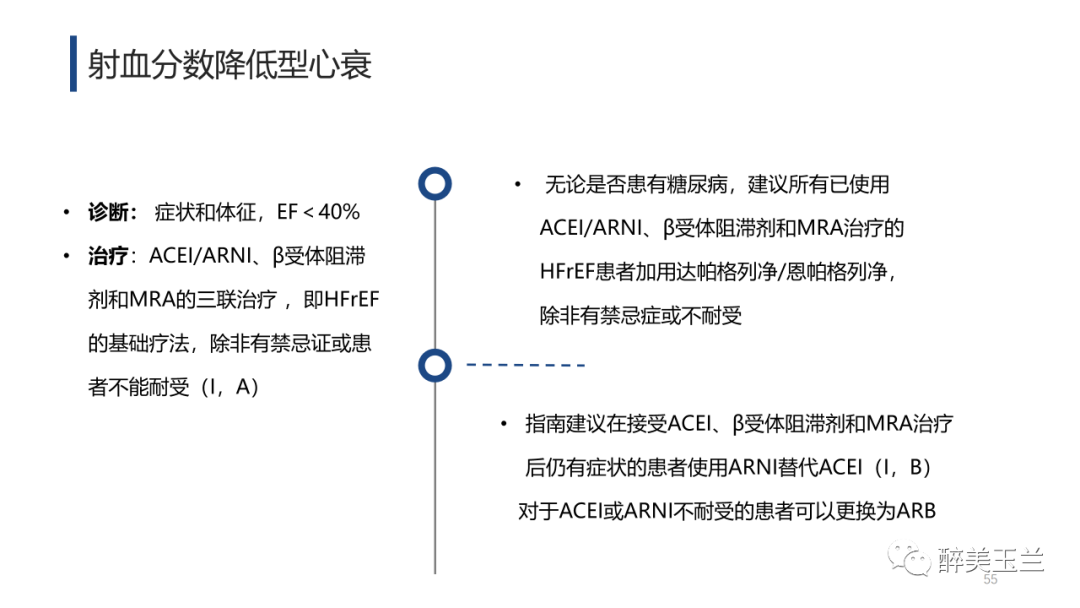
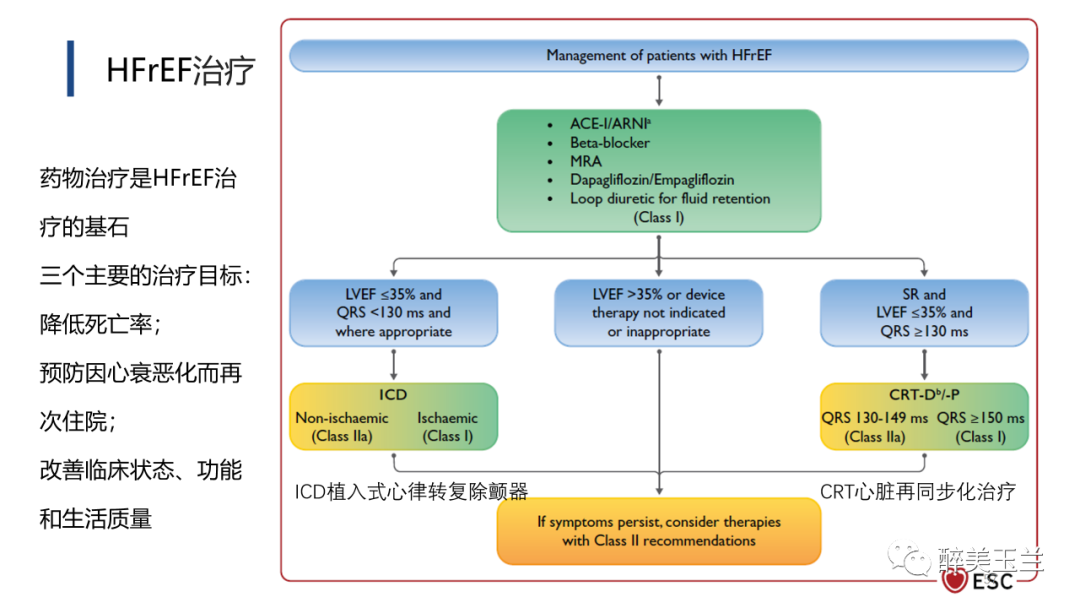
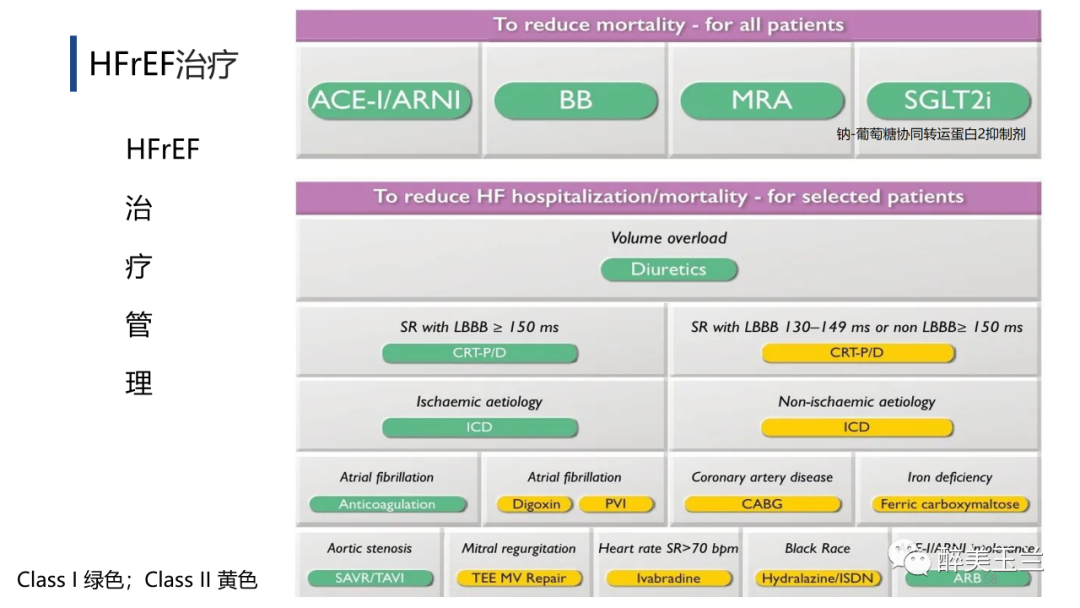
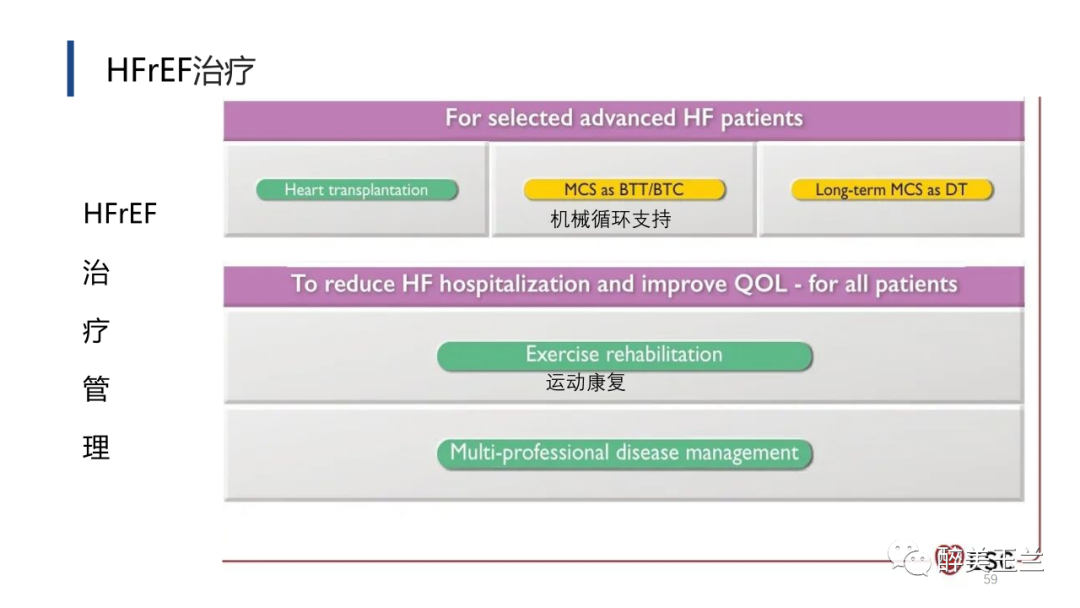
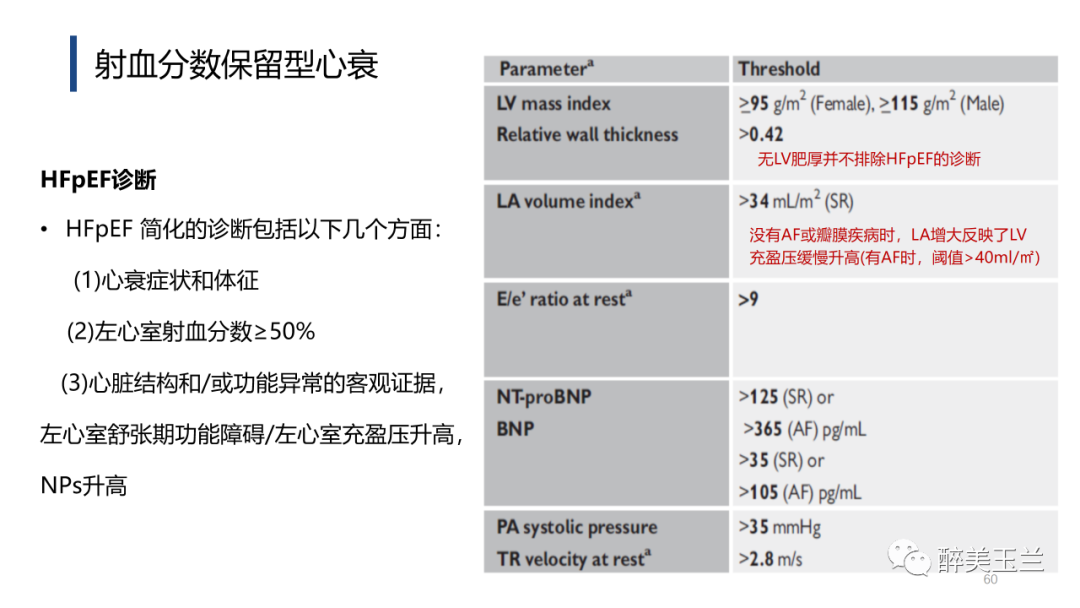
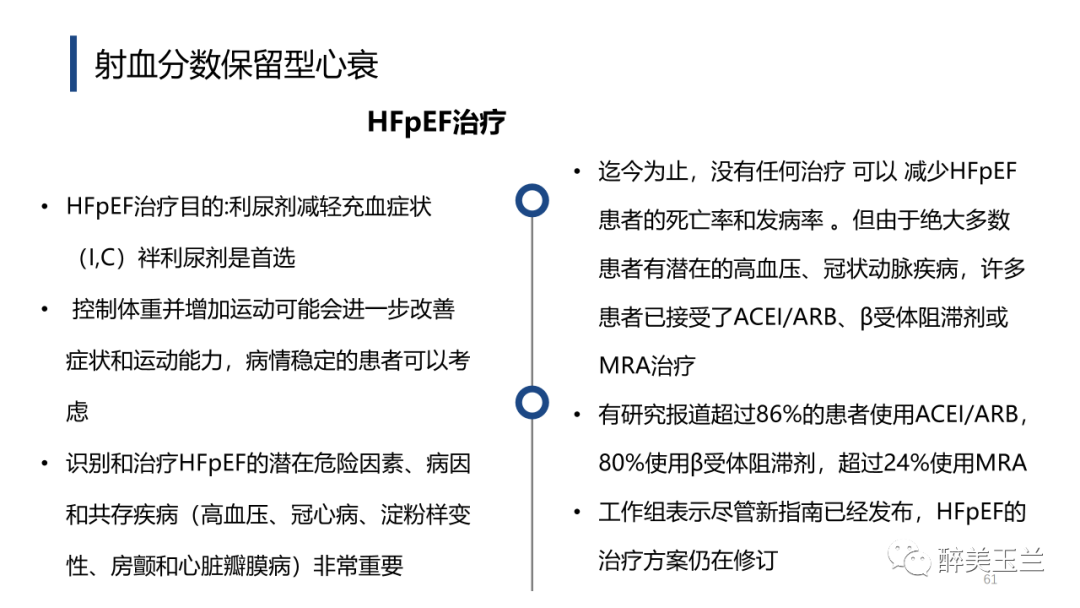
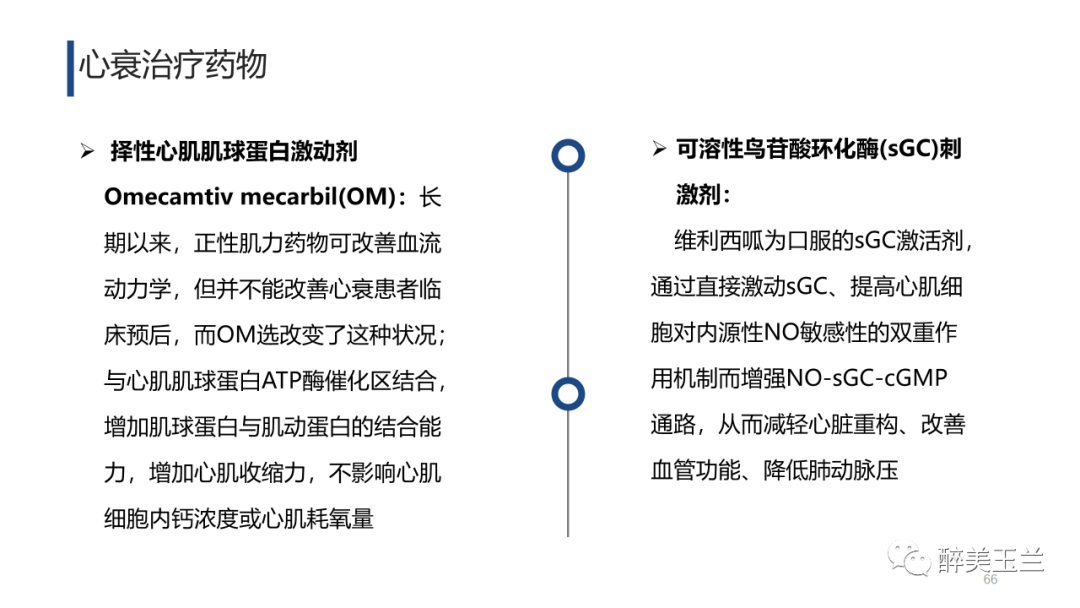
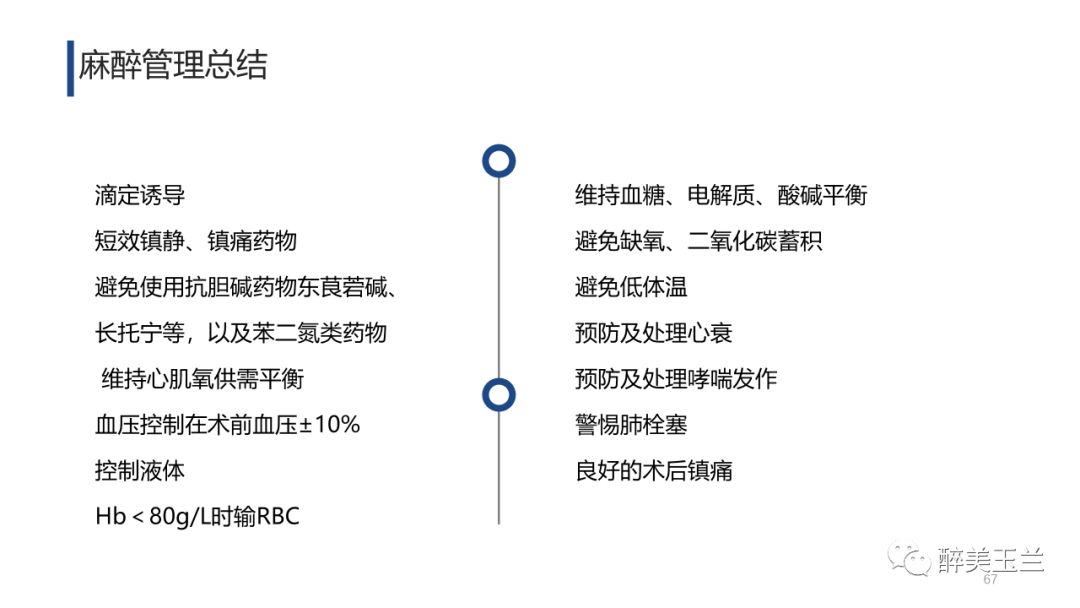
心衰是由心脏结构/功能异常引起相应症状/体征的一种综合征,患病率随着年龄的增长而增加:<55岁的患病率约1%>10%;根据EF值分将心衰分为三种类型:为HFrEF(EF≤40%)、HFmEF(41%≤EF≤49%)、HFpEF(EF≥50%) ,本次病例为大家分享了老年心衰患者PFNA术中关注要点及心衰的部分解读 。





小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了
36
学习了
30
#病例讨论#
39
#FNA#
44
写的很好。知识更新的好多。谢谢
56
#心衰患者#
47
#内固定#
51