『疼痛』对于人类而言,如同敌人一样存在着,它总是折磨着你吃不好,睡不好,无法正常生活。当药物治疗无效时,我们需要进行『疼痛微创治疗』,虽然它可以有效的缓解疼痛,但是万万不可轻视它可能出现的并发症:局『麻药全身毒性(LAST)』。
随着影像引导技术的发展,临床医生经验的累积,LAST的发生率已经很低了,但是低不等于零,这仍是一种危及生命的并发症。
比如今日这位中年女性患者,在进行疼痛微创治疗后出现了心动过速、呼吸急促和缺氧等危机症状。究竟是发生了什么呢?
这是一位有『多发性骨髓瘤(MM)』病史的女性患者,伴有高钙血症和慢性骨痛。多模式镇痛方案和大剂量阿片类药物已经无法控制她的疼痛,因严重的急性疼痛危象入院。
由于疼痛剧烈,患者无法忍受脊柱磁共振(MRI)检查,因此决定MRI之前先进行疼痛介入治疗,以便能够顺利的完成脊柱MRI检查。于是在疼痛门诊X线引导下在L4-L5节段置入硬膜外导管用于姑息疼痛治疗(如图1)。
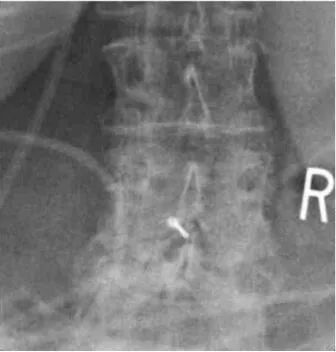
图1:X线引导下L4-L5节段置入硬膜外导管
局部使用2ml利多卡因逐层浸润,在确认导管位置后,给予3ml的1%利多卡因和肾上腺素的试验剂量,心率没有发生变化,于是从导管输注8ml的0.25%布比卡因。
进行15分钟的监测后,转移至MRI检查区域,计划在检查之后开始持续的硬膜外药物输注。
在此期间,患者发生LAST,出现心动过速,高血压,呼吸急促,缺氧,SpO2为83%,需要进行气道正压通气。患者被紧急转移到ICU。左侧胸腔穿刺置管引流,排出1L胸水,无并发症发生,并持续滴注利多卡因。
大约15分钟后,与治疗前心电图(如图2)相比,新出现左束支传导阻滞(如图3)。在接下来的20分钟内,患者出现了轻微的心血管系统反应。
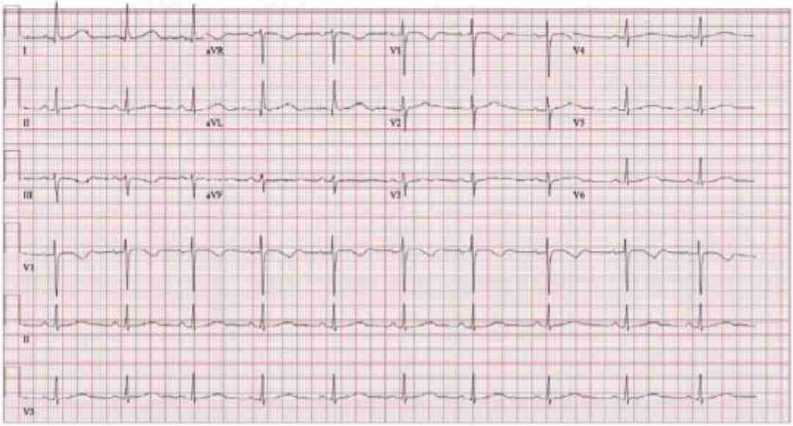
图2:治疗前心电图
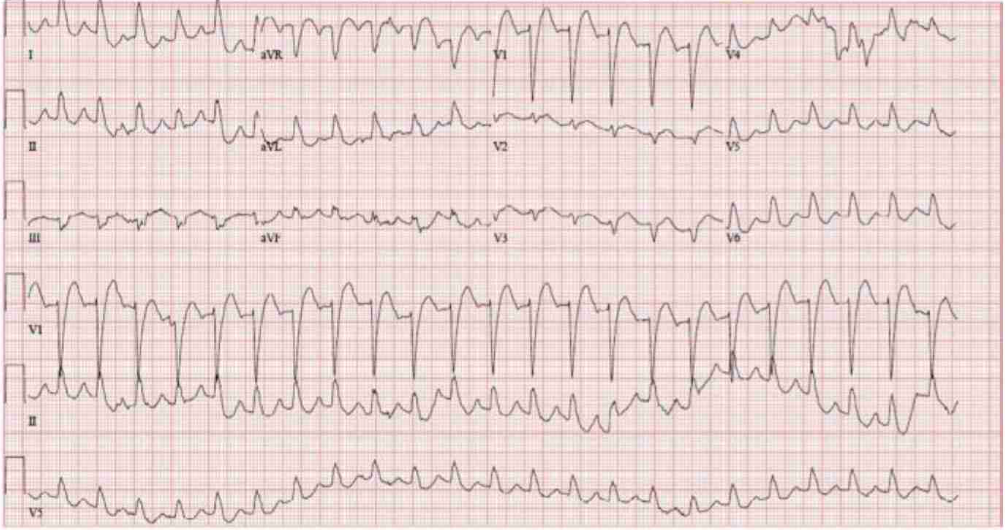
图3:并发局麻药全身毒性后心电图
在患者近期化疗过程中,使用了类固醇类激素,同时给予了大剂量正性肌力药和血管升压药(多巴酚丁胺10ug/kg/min,肾上腺素0.2ug/kg/min,去甲肾上腺素0.3ug/kg/min,加压素0.04U/min)。
在全身运动功能减退的情况下,超声心动图显示左心室射血分数(LVEF)只有25-30%(正常值为50-70%),未发现局部的心室壁运动异常。
考虑到患者严重的,难以维持的血流动力学障碍和既往使用过布比卡因的情况,LAST发生后先用1.5ml/kg静脉滴注20%脂乳剂,再0.25ml/kg/min静脉滴注,即刻缓解显著。
不久后,患者几乎停止了所有血管活性药物,并且精神状态良好。复查心电图显示窦性心律(如图4)。初次检查TTE后进行复查,双心室功能恢复且LVEF为50%。
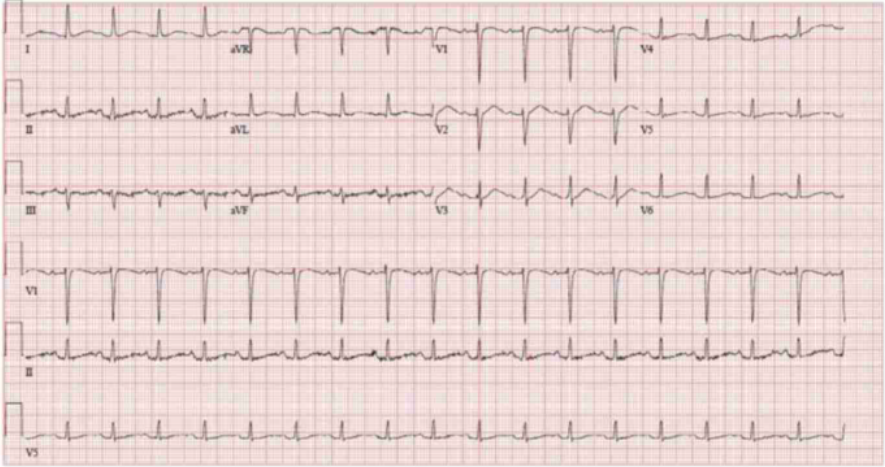
图4:滴注脂肪乳剂后心电图恢复窦性心律
最终检查结果显示所有椎体和肋骨广泛性溶骨病变明显加重,与弥漫性骨髓瘤病情一致。此外,L4-L5背侧软组织及L3-L4右侧水平有皮下结节,与皮肤骨髓瘤病情一致(如图5)。

图5:可见椎体中出现多处溶骨性病变
『局麻药全身毒性(LAST)』是可危及生命的并发症,在周围神经阻滞中发生率为2.5-9.8/10000,在硬膜外麻醉中发生率为1.2-11次/10000。
患者病情进展和恢复时间线如下所示(如图6)。
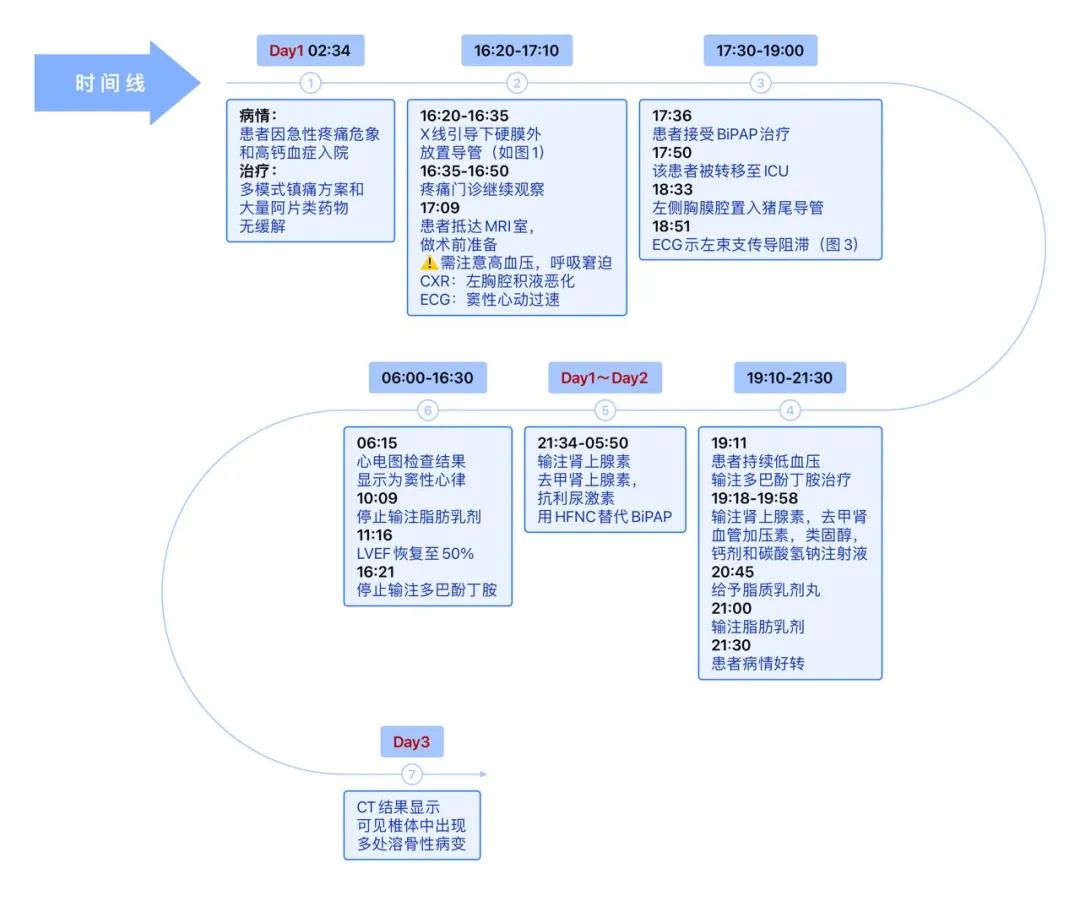
图6:病情进展和恢复的时间线

在该病例中,导致心血管系统衰竭的局麻药全身毒性是非常罕见的,但在这种情况下,可能存在潜在的病因。LAST的风险随着局麻药用量、低体重、极限年龄和预先存在的心脏、肝脏、肾脏和代谢功能障碍而增加。
该女性所患原发病:多发性骨髓瘤(MM),也会导致LAST的易感性增加。典型的MM包括肾脏损害,神经病变,静脉血栓栓塞,肝脏受累和溶骨性骨病变。
活跃的MM伴骨髓微血管密度显著增加引起组织代谢紊乱。在本例患者中,CT上可见所有椎体和皮肤骨髓瘤区域的溶解性病变,可能与血管床增加有关。

在任何肿瘤病变部位附近进行局麻药操作都有可能增加LAST的风险,因此需要高度警惕。那么该如何降低LAST发生的风险呢?临床医生可以考虑仅使用阿片类药物向神经周围注射,此外也可选用1%苯海拉明或苯甲醇作为局部浸润的代替药物。
此外,建议在硬膜外和周围神经阻滞注射时使用含有肾上腺素的试验剂量,局麻药避免使用布比卡因,并延长连续监测时间以此来降低使用剂量,从而降低LAST发生的风险。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学到了
35
#多发性#
46
#局麻#
39
签到学习
43
#多发性骨髓瘤#
83
这个研究不错,厉害了!!!谢谢分享
45
***,谢谢
42
认真***
59