Nat Med:持续实验和临床疼痛的神经影像生物标记物
2021-03-05 MedSci原创 MedSci原创
Choong-Wan Woo等发现一种可用于鉴别持续性疼痛实验和临床特沟通的神经影像生物标志物。
持续性疼痛是临床疼痛障碍的一个主要特征,但很难从患者的认知和情感特征中单独进行评估。
疼痛是一个重大的临床和社会问题。五分之一的美国成年人(20.4%)目前患有临床疼痛,每年的经济成本高达数千亿美元。临床疼痛的一个重要特征是其持续性,除了感觉辨别过程外,它还可能涉及与自上而下的认知和情感应对反应相关的大脑区域。然而,由于临床疼痛通常受到多种因素的影响,如学习和评价、情绪和情绪以及注意力和自我参照过程,因此客观地评估患者的持续性疼痛仍然是困难的。强直性实验性疼痛长期被用作临床疼痛的实验模型,它与临床疼痛具有相似的特征。紧张性疼痛和临床性疼痛都是在较长的时间范围内展开的,比实验性相性疼痛(EPP)更令人不快,更有可能引发自发的应对反应。相比之下,EPP持续的时间较短,在性质和神经生物学上都与临床疼痛和紧张性疼痛不同。这增加了紧张性疼痛可能在神经生物学上更接近于持续的临床疼痛的可能性。然而,以前的人类神经影像研究没有直接研究强直性实验疼痛、相位性实验疼痛和临床疼痛之间的神经表现有何相似或不同之处。
Choong-Wan Woo等发现一种可用于鉴别持续性疼痛实验和临床特沟通的神经影像生物标志物,发表在Nat Med杂志。
在这项研究中,该团队开发了一种基于全脑功能连接的功能性磁共振成像信号,跟踪实验诱导的紧张性疼痛强度,并通过六项研究(总共n=334项)测试了其对临床疼痛的敏感性、特异性和概括性。通过三项关于口腔面部紧张性疼痛和厌恶味觉的独立研究,该特征对紧张性疼痛表现出高度的敏感性和特异性。它还预测了临床疼痛的严重程度,并在两项关于临床下腰痛的独立研究中对患者和对照组进行了分类。
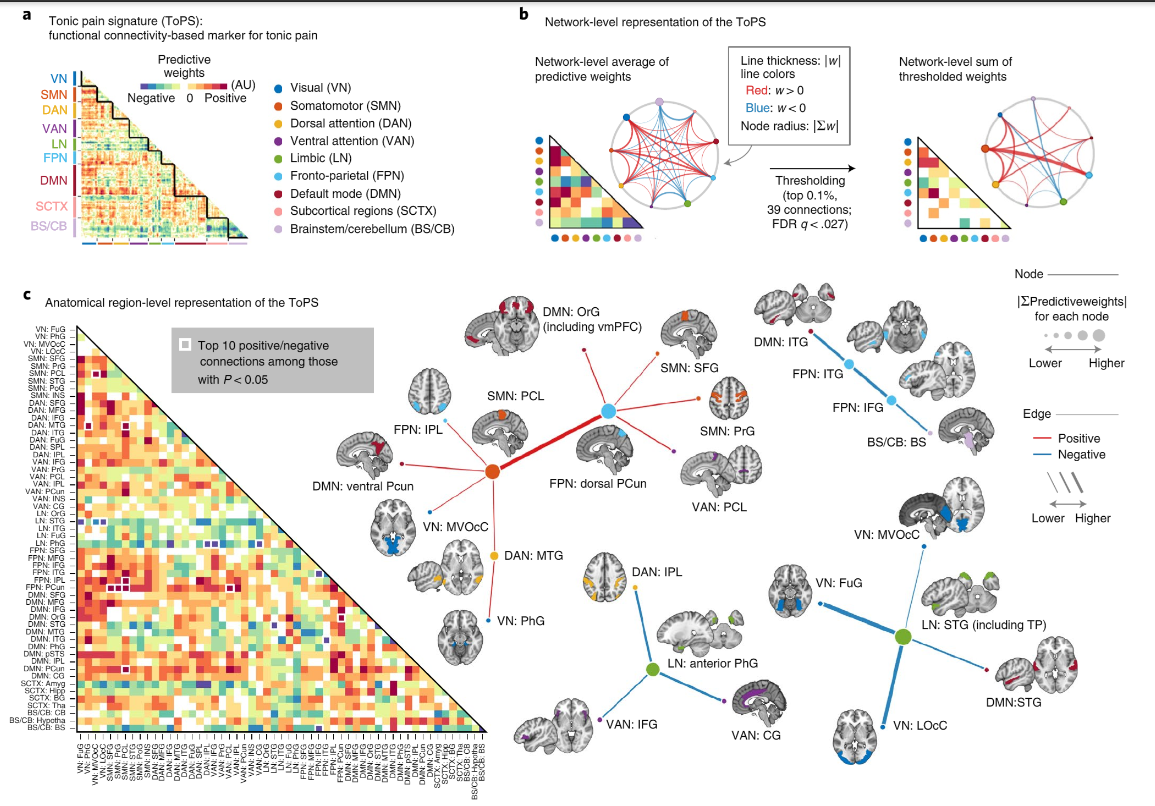
TOPS:紧张性疼痛的功能性连接标记。A、模型的原始预测权重。根据大脑区域的功能网络成员对它们进行排序。B,左:平均每个网络的顶部预测权重,并用一个下三角矩阵和一个圆形图来显示它们。右图:在网络水平对基于10,000次迭代的Bootstrap测试的前0.1%阈值权重求和(P<0.000028,经FDR校正的Q<0.027,双尾)。C,将地块分成每个功能网络内的大体解剖区域,并平均每个解剖区域内的预测权重。用Bootstrap测试(左侧两个白框拖尾)显示前10个正负连接以及在未校正的P<0.05阈值下存活的相应脑区。
紧张性疼痛和临床疼痛显示出相似的网络水平表现,特别是在躯体运动、额顶和背部注意网络中。这些模式与实验性阶段性疼痛的表现截然不同。这项研究确定了一个具有很高临床转译潜力的持续性疼痛的脑生物标志物。
总体而言,这种基于功能连接的紧张性疼痛信号,具有临床转译的潜力。虽然还需要对来自不同人群和不同实验室的数据进行进一步的验证和独立测试,才能为其稳健性和普适性提供更确切的证据,但该研究的八个独特研究队列的概括性的研究结果为向能够定量评估持续疼痛的神经成像疼痛生物标记物迈出了有意义的一步。
原文出处:Lee Jae-Joong,Kim Hong Ji,Čeko Marta et al. A neuroimaging biomarker for sustained experimental and clinical pain.[J] .Nat Med, 2021, 27: 174-182.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#标记物#
28
#神经影像#
40
#Nat#
37
#生物标记#
43
#生物标记物#
36
#Med#
32