创新药物可及性不断提升,助力中国肺癌患者生存获益
2021-01-20 kathy 医谷网
如今,肺癌已成为“癌症第一杀手“。据人民日报发布的“2018年全球癌症数据”显示,肺癌全球发病率和死亡率分别占全部恶性肿瘤的11.6% 及18.4% ,是全球发病率和死亡率最高的癌症。
如今,肺癌已成为“癌症第一杀手“。据人民日报发布的“2018年全球癌症数据”显示,肺癌全球发病率和死亡率分别占全部恶性肿瘤的11.6% 及18.4% ,是全球发病率和死亡率最高的癌症。在中国,肺癌同样是中国发病率、死亡率最高的癌症。随着近年来肺癌诊疗技术的长足发展和疾病认知水平的不断提高,以及药物可及性的持续加强,中国肺癌患者的生存时间和生活质量已经得到了明显改善。
治疗策略不断优化,肺癌向慢病变迁
根据组织病理学特点不同,肺癌可分为非小细胞肺癌(NSCLC)和小细胞肺癌(SCLC) ,其中绝大多数是非小细胞肺癌,包括鳞癌、腺癌、大细胞癌,约占所有肺癌的80%-85% ,约75%的患者在发现时已处于中晚期,5年生存率极低 。
目前肺癌常见的治疗方式包括手术、放疗、化疗、靶向治疗、免疫治疗等,其中靶向治疗和免疫治疗的出现开创了肺癌治疗新纪元,使得越来越多的肺癌患者凭借着创新药物获得了长期生存和更高的生活质量,打破了人们对肺癌治疗的传统认知。
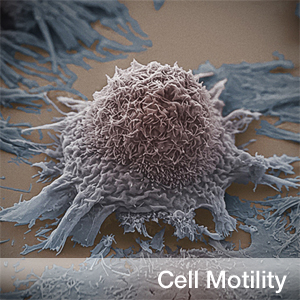
所谓靶向治疗就是针对已经明确的致癌位点,使用不同的靶向药物来阻断癌细胞的信号传导,阻碍癌细胞生长,具有全身副反应小,作用精准、效果优越的特点。患者需要进行基因检测来确定是否有相关的靶点基因改变来选择靶向治疗方法。目前研究比较透彻的靶点包括EGFR、ALK、ROS1等,随着二代测序技术在临床上的广泛应用,越来越多的突变率较低的肺癌罕见靶点被发现,如c-Met、Her-2、RET等。
据复旦大学肿瘤医院放疗中心、肺癌中心副主任、复旦大学胸部肿瘤研究所副所长樊旼教授介绍:“与其他国家相比,我国的肺癌有着独特的流行病学特征和患者类型,比如我国肺腺癌患者的EGFR(表皮生长因子受体)突变率约为60%,而美国仅为10%左右,正是这种区别于别国的高基因突变率,使得靶向治疗在中国越来越受到临床医生的重视,成为目前中国肺癌诊疗的重要手段之一。”
樊旼教授表示,对于靶向治疗,患者通常关注的是能否获益,治愈的可能性,耐药问题和医保报销问题。“医生通常会根据患者的靶标、分期以及身体状况来选择靶向治疗方案。中晚期患者不代表没有治愈的可能,我们发现转移次数相对较少的晚期患者采用化疗联合靶向治疗方案比单纯采用靶向治疗能够获得更好的疗效。耐药是常见的情况,可以使用不同的药物组合在不同的时期获得最大的效果。”
“目前已有针对不同靶点的肺癌靶向药物相继在我国上市,EGFR、ALK等常见的靶点已经有一代、二代、三代靶向药物‘三代同堂’,使得肺癌患者无论是一线、二线、甚至是三线治疗都有对应的药物可以选用,不断帮助患者延长生存期。据最新临床研究显示,EGFR阳性晚期非小细胞肺癌患者一线使用三代原研靶向药的总生存期达到了38.6个月,超过了3年。越来越多肺癌患者可以带癌长期生存,肺癌正在逐步向慢病化转变。” 樊旼教授说道。
提升创新药物可及性是患者能够长期获益的关键
如果说药物不断创新及治疗策略的不断优化,为肺癌的长期生存带来了希望,那么提升药物可及性才是实现这一目标的关键。创新药物上市初期,由于研发成本、专利等因素,价格往往会比较高,使得很多经济能力有限的患者望而却步,有些患者不得不放弃最佳治疗方案。为了推动创新药物的可及性,充分满足患者的用药需求,近年来,我国持续进行国家医保目录的谈判准入和更新工作,使得越来越多的优质创新药物被纳入医保目录,越来越多的患者从中获益。
2021年元旦前,《国家基本医疗保险、工伤保险和生育保险药品目录(2020年)》正式公布,并将于今年3月1日起正式实施。目录内药品总数2800种,其中西药1426种,中成药1374种。药饮片未作调整,仍为892种。本次医保目录调整,共对162种药品进行了谈判,119种谈判成功,谈判成功率为73.46%,谈判成功的药品平均降价50.64%。 在肿瘤领域,有超过50种抗肿瘤药被纳入医保,其中和肺癌患者有关的有7种靶向药物和2种免疫药物。
樊旼教授表示:“经济因素是影响患者治疗依从性的关键。此次新版医保目录的更新,将更多疗效确切的好药和最新适应症及时纳入医保,使得中国晚期肺癌患者能以低廉的价格用上与国际同步的创新药物和治疗方案,兼顾了最佳疗效和最优价格。甚至获得国内外权威指南一致推荐的三代靶向药的一线疗法也被纳入医保,大大减轻了患者的经济负担。我们也期待未来能够有更多创新药物进入医保,惠及更多患者。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#肺癌患者#
54
#新药物#
39
#可及性#
44
👌
71
#患者生存#
42
#生存获益#
43
#创新#
37