NEJM:II 期结肠癌患者化疗决策新指标!化疗可免,生存照旧?
2022-06-17 MedSci原创 MedSci原创
N Engl J Med:循环肿瘤DNA分析指导II期结肠癌辅助治疗
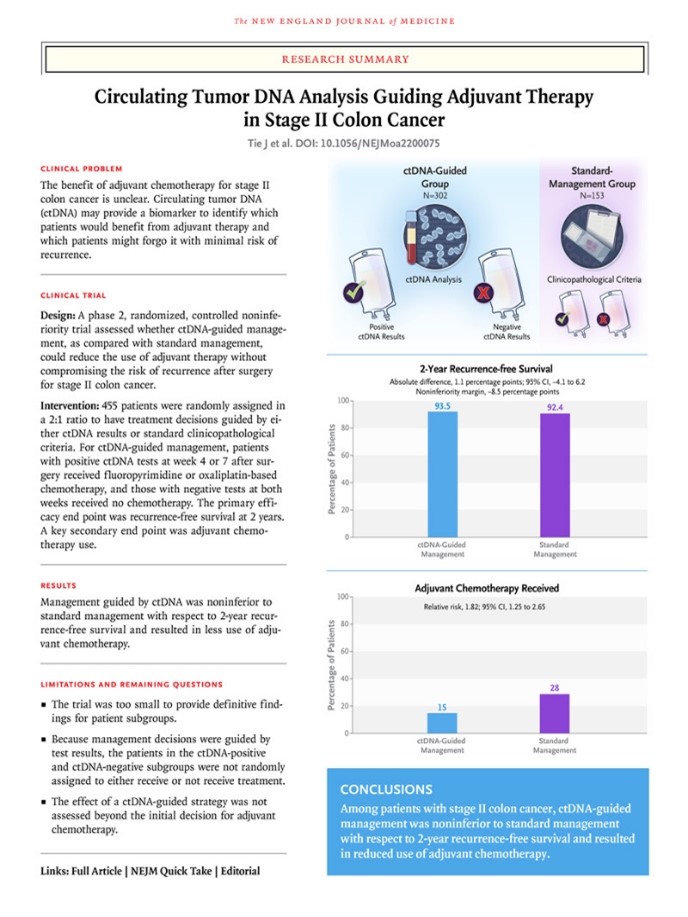
辅助化疗在 II 期结肠癌中的作用仍存在争议。肿瘤循环DNA (ctDNA)的存在预示着术后无复发生存率极低,而其不存在则预示着复发风险较低。对ctdna阳性患者进行辅助化疗的益处尚不十分清楚。

本研究进行了一项试验,旨在评估ctDNA引导的方法是否可以在不影响复发风险的情况下减少辅助化疗的使用。II期结肠癌患者以2:1的比例随机分配,根据ctDNA结果或标准临床病理学特征指导治疗决策。对于 ctDNA 引导下的治疗,术后 4 或 7 周的 ctDNA 阳性结果提示以奥沙利铂或氟嘧啶为基础的化疗。ctDNA阴性的患者未接受治疗。主要疗效终点是 2 年时无复发生存率。一个关键的次要终点是辅助化疗的使用。

结果显示,在455例接受随机分组的患者中,302例被分配到ctDNA引导下治疗,153例被分配到标准治疗。中位随访时间为37个月。与标准治疗组相比,ctDNA引导组接受辅助化疗的患者比例较低(15% vs 28%;相对风险,1.82;95%可信区间[CI],1.25-2.65)。在评估 2 年无复发生存率时,ctDNA 引导下治疗不劣于标准治疗(分别为 93.5% 和 92.4%;绝对差异为 1.1 个百分点;95% CI,−4.1 至 6.2 [非劣效性边界,−8.5 个百分点])。在接受辅助化疗的 ctDNA 阳性患者中,3 年无复发生存率为 86.4%,在未接受辅助化疗的 ctDNA 阴性患者中,三年无复发生存率为 92.5%。
研究结果表明, ctDNA 引导的 II 期结肠癌治疗方法减少了辅助化疗的使用,但并不会影响无复发生存期。
原文来源:
Tie J, Cohen JD, Lahouel K, Lo SN, Wang Y, Kosmider S, Wong R, Shapiro J, Lee M, Harris S, Khattak A, Burge M, Harris M, Lynam J, Nott L, Day F, Hayes T, McLachlan SA, Lee B, Ptak J, Silliman N, Dobbyn L, Popoli M, Hruban R, Lennon AM, Papadopoulos N, Kinzler KW, Vogelstein B, Tomasetti C, Gibbs P; DYNAMIC Investigators. Circulating Tumor DNA Analysis Guiding Adjuvant Therapy in Stage II Colon Cancer. N Engl J Med. 2022 Jun 16;386(24):2261-2272. doi: 10.1056/NEJMoa2200075. Epub 2022 Jun 4. PMID: 35657320.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#决策#
0
#学习##期刊论坛#
63
不错的文章
50
NEJM上果然牛,感谢梅斯更新及时
30