JAMA:卡瑞丽珠单抗联合化疗一线治疗明显改善晚期食管鳞状细胞癌患者的预后:3期临床研究ESCORT-1st
2021-09-15 yd2015 MedSci原创
该研究表明,卡瑞丽珠单抗联合化疗一线治疗明显改善晚期食管鳞状细胞癌患者的预后。
食管癌是中国常见的恶性肿瘤之一,在流行病学、遗传背景、病理分型等多个方面,中国食管癌都与欧美等国存在差异。近两年,免疫治疗在食管癌二线治疗中取得成功,推动了食管癌免疫治疗时代的到来。昨日,JAMA杂志发表由中山大学肿瘤防治中心徐瑞华教授牵头的3期临床研究ESCORT-1st结果。该结果的发表,将免疫治疗前移至食管癌一线治疗,将有可能改变临床实践。
ESCORT-1st研究是在全国60多家中心开展的随机、双盲、安慰剂对照、III期临床研究,旨在评估卡瑞利珠单抗联合紫杉醇和顺铂对比安慰剂联合紫杉醇和顺铂用于晚期食管癌一线治疗的有效性和安全性。
研究最终纳入596例患者,卡瑞丽珠单抗联合化疗组和化疗组各298例。中位随访时间为10.8个月(7.3-14.3个月)。独立评估委员会评估,卡瑞丽珠单抗联合化疗组较化疗组明显改善患者的中位总生存期(OS),分别为15.3个月 [95% CI, 12.8-17.3]和12.0个月[95%CI,11.0-13.3](HR=0.70,95% CI, 0.56-0.88;单侧P = 0.001)。
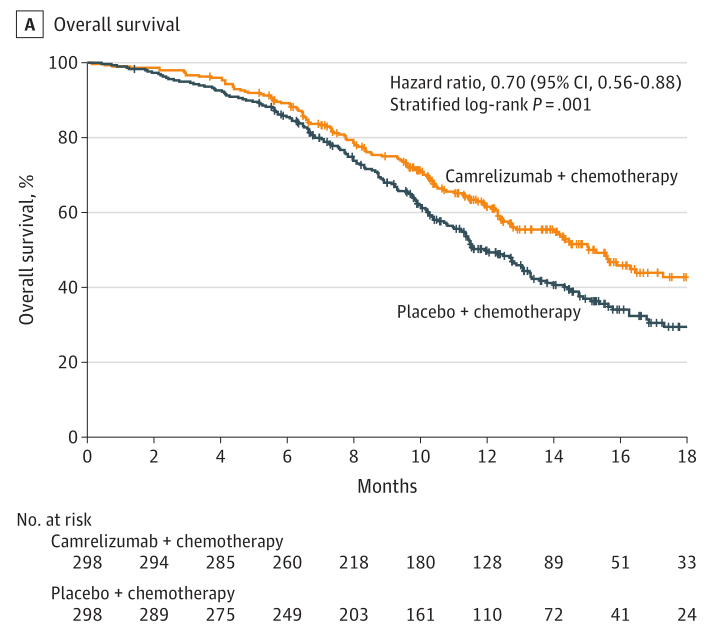
OS
同样,卡瑞丽珠单抗联合化疗组较化疗组明显改善患者的中位无进展生存期(PFS),分别为6.9个月[95% CI, 5.8-7.4]和5.7个月[95% CI, 5.5-5.7](HR= 0.56, 95%CI,0.46-0.68; 单侧P <0.001)。

PFS
联合组和单用化疗组的6个月,12个月,18个月的生存率分别为89.2%(95%CI,85.1%-92.2%) vs 85.5% (95% CI, 80.9%-89.0%); 61.5% (95% CI, 55.4%-67.1%) vs 49.8% (95% CI, 43.6%-55.6%); 42.7% (95% CI, 35.3%-50.0%) vs 29.5% (95% CI, 22.9%-36.3%)。
两组的ORR分别为72.1% (95% CI, 66.7% to 77.2%)和62.1%(95% CI,56.3% to 67.6%)( 2-sided P = 0.009);两组的疾病控制率(DCR)分别为91.3% (95% CI, 87.5% to 94.2%)和88.9% (95% CI, 84.8% to 92.3%)( 2-sided P =0.33)。
两组治疗相关严重不良事件分别发生在296例患者(99.3%)和288例患者(97.0%)中;而两组≥3级治疗相关不良事件分别发生在189例患者 (63.4%)和201例患者(67.7%)中,包括治疗相关性死亡分别有9例患者 (3.0%)和11例患者(3.7%)。

不良事件
综上,该研究表明,卡瑞丽珠单抗联合化疗一线治疗明显改善晚期食管鳞状细胞癌患者的预后。
原始出处:
Luo H, Lu J, Bai Y, et al. ESCORT-1st Investigators. Effect of Camrelizumab vs Placebo Added to Chemotherapy on Survival and Progression-Free Survival in Patients With Advanced or Metastatic Esophageal Squamous Cell Carcinoma: The ESCORT-1st Randomized Clinical Trial. JAMA. 2021 Sep 14;326(10):916-925. doi: 10.1001/jama.2021.12836. PMID: 34519801.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#细胞癌#
29
#3期临床#
52
#食管鳞状细胞癌#
51
#联合化疗#
33
#食管#
28
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
56