EuroIntervention:肾动脉超声消融治疗难治性高血压长期随访结果公布(RADIANCE-HTN SOLO研究)
2021-07-25 MedSci原创 MedSci原创
早期研究表明,射频去肾交感神经术可降低中度高血压患者的血压。我们研究了在不给予降压药物的情况下,一种替代技术——血管内超声肾交感神经消融术是否能降低高血压患者的动态血压。
早期研究表明,射频去肾交感神经术可降低中度高血压患者的血压。我们研究了在不给予降压药物的情况下,一种替代技术——血管内超声肾交感神经消融术是否能降低高血压患者的动态血压。
RADIANCE-HTN 是一项随机、双盲、假手术对照、2队列研究( TRIO 和 SOLO ),旨在证明Paradise 导管系统在两组不同高血压受试者中的有效性和安全性。使用1种或2种降压药物可控制的原发性高血压患者或使用0-2种降压药物难以控制的原发性高血压患者将被纳入RADIANCE Solo队列,而至少使用3种降压药物治疗的难治性高血压患者将被纳入RADIANCE Trio队列。在随机分组之前,受试者在不服用降压药物治疗的情况下(SOLO)或尽管采用稳定的、单片、三联、固定剂量的复方降压药物治疗方案(TRIO),仍无法控制高血压。详细:Lancet:肾动脉超声消融治疗难治性高血压效果明显(RADIANCE-HTN TRIO研究)
其中,RADIANCE-HTN SOLO是一项多中心、国际性、单盲、随机、假手术对照试验,在美国21个中心和欧洲18个中心进行。年龄18–75岁双期高血压,停用降压药(0~2种)4周后动态血压≥135/85 mm Hg且170/105 mm Hg且肾动脉解剖符合手术条件。
患者随机(1∶1)分为用 Paradise系统进行肾交感神经消融术(ReCor Medical, Palo Alto, CA, USA)及假手术(仅进行肾血管造影)。随机化序列是计算机生成的,并依据中心进行分层,每层由4~6个随机区组组成,每个区组有不同的治疗组合。患者和结果分析员对随机化过程不知情。
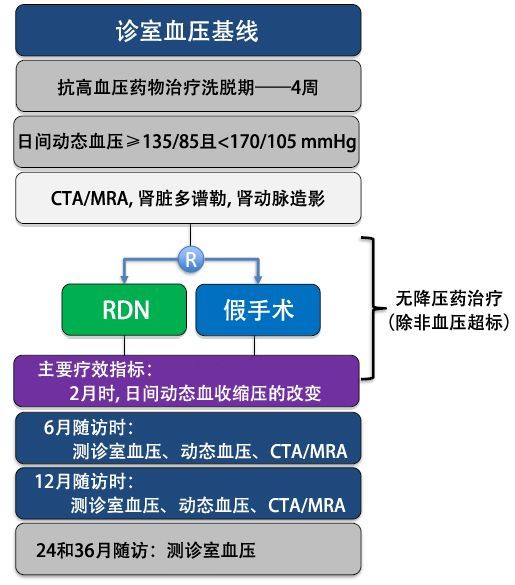
主要疗效终点是意向治疗人群2个月时日间动态收缩压的变化。除非超过预定定的血压标准,否则患者在整个2个月的随访期间患者应停用抗高血压药物。主要不良事件包括全因死亡率、肾功能衰竭、伴有终末器官损伤的栓塞事件、需要治疗的肾动脉或其他主要血管并发症、30天内因高血压危象入院以及6个月内新发肾动脉狭窄。本研究注册于ClinicalTrials.gov,编号NCT02649426。
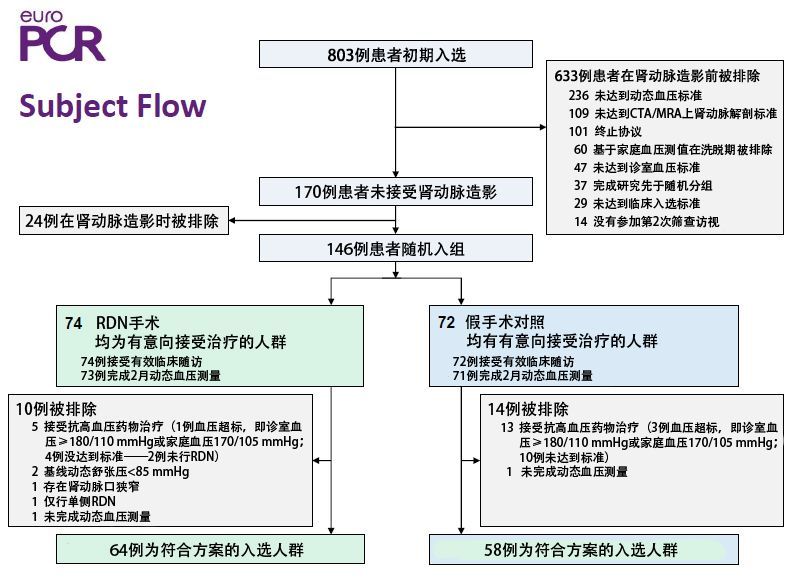
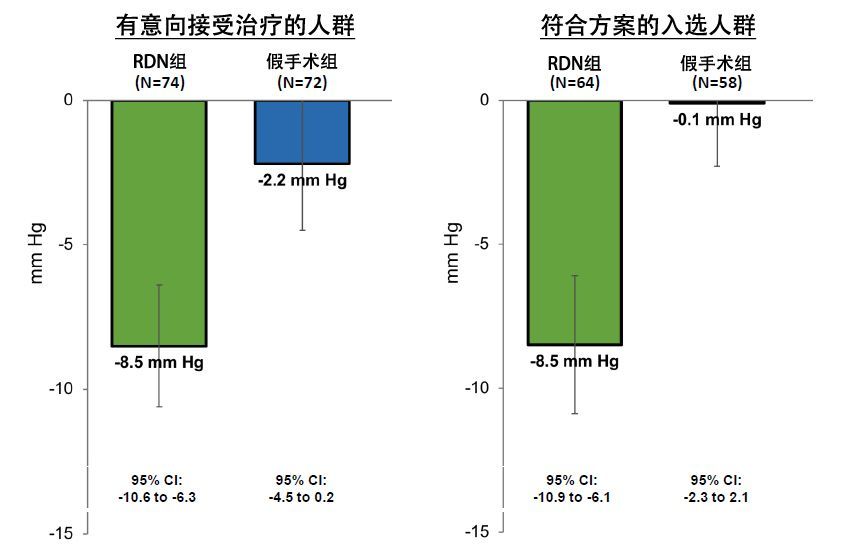
结果显示,2016年3月28日至2017年12月28日期间,共筛选了803例合格的患者,146例患者随机接受肾交感神经消融术(n=74)或假手术(n=72)。去肾交感神经术组(−8·5 mm Hg, SD 9·3)的白天动态收缩压降低幅度大于假手术组(−2·2mm Hg, SD 10·0; 基线校正组间差异: −6·3 mm Hg, 95% CI −9·4 to−3·1, p=0·0001)。两组均未报告重大不良事件。
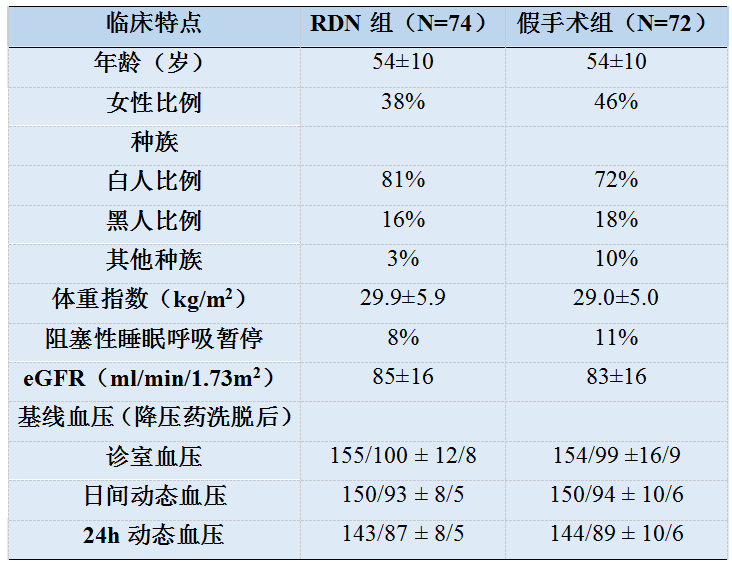
两组患者基线资料对比
术后2个月随访时,RDN组与假手术组主要疗效终点
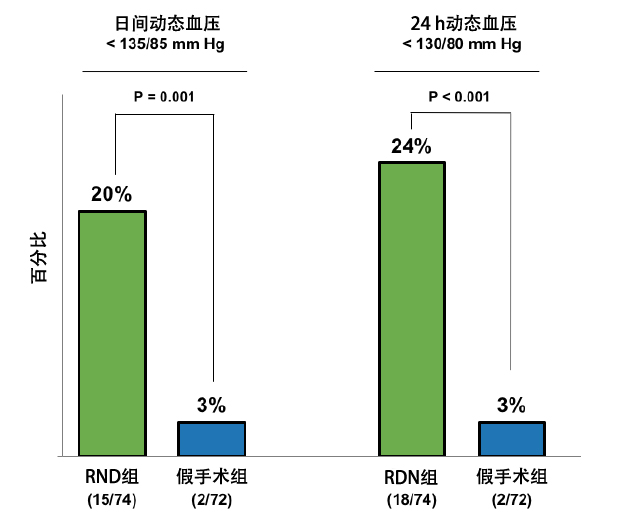
比较两组患者个体化降压反应发现,日间动态收缩压降幅≥5mmHg的患者在RDN组和假手术组中分别占66%和33%(P <0.001)(Figure 5);两组无降压药条件下的血压达标率分别为20%和3%(P <0.001)(Figure 6)。在安全性方面,两组术后30d内均未出现主要不良事件(死亡、急性肾衰竭、致器官损伤的血栓事件、需干预的血管并发症、高血压危象和肾动脉狭窄>70%)。
随访2个月时,患者的个体血压反应情况
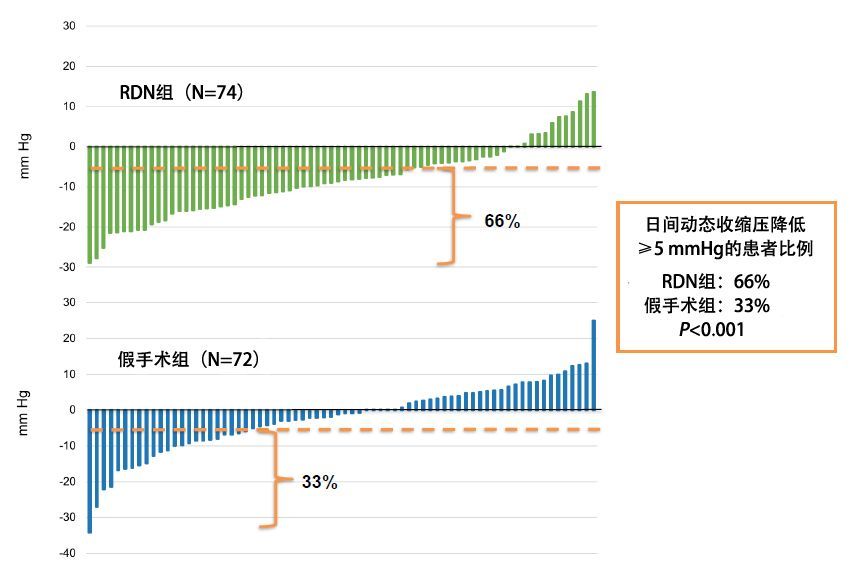
Figure 6
无降压药条件下的血压控制率
与假手术相比,在无药物治疗的情况下,血管内超声去肾交感神经术可减少收缩压舒张压同时升高的高血压患者2个月时的动态血压。
12个月的随访结果显示,74 名 RDN 患者中的 65 名和 72 名假手术患者中的 67 名进行了 12 个月的 dASBP 测量。 使用≥2 种药物的患者比例(27.7% 对 44.8%;p = 0.041)、药物数量(0 对 1.4;p = 0.015)和定义的每日剂量(1.4 对 2.2;p = 0.007) 与 RDN 相比,sham组 较少。 RDN 组 dASBP 从基线下降 (-16.5 ± 12.9 mm Hg) 在 12 个月时保持稳定。 12 个月时 RDN 与假调整后的差异为 -2.3 mmHg(95% 置信区间 [CI]:-5.9 至 1.3mmHg;p = 0.201)对于 dASBP,-6.3 mmHg(95% 置信区间:-11.1 至 - 1.5 mmHg;p = 0.010)对于办公室 SBP,和 -3.4 mmHg(95% CI:-6.9 至 0.1 mmHg;p = 0.062)对于家庭 SBP。 RDN 组中 SBP 的访问间变异性较小。 计算机断层扫描或磁共振血管造影未检测到肾动脉损伤。
最新发表在EuroIntervention上结果显示,在假手术组的 72 名受试者中,33 名在平均随访 23±6 个月后接受了超声 RDN。 在交叉之前,患者的白天动态血压为 144.1±10.1/89.9±8.4 mmHg,并接受了 1.2±0.8 种降压药物。 从交叉前到 RDN 后 2 个月和 6 个月,白天动态血压的平均变化为 -11.2±13.7/-7.1±8.9 mmHg(n=33;p<0.001;p<0.001)和 -10.8±17.3/-7.8± 11.6 mmHg(n=27;p=0.002;p<0.001)。 从交叉前基线到 2 个月和 6 个月,抗高血压药物的数量没有变化。 33 名患者中的 18 名 (54.5%) 在 RDN 后 2 个月和 6 个月时控制了他们的日间动态血压 (<135/85 mmHg) 和 44.4% (12/27)。 没有发生与手术相关的重大不良事件。
肾动脉去交感神经消融术的复苏
经导管RDN是一项颇具吸引力而又饱受争议的技术,在高血压、心力衰竭、难治性电风暴,甚至房颤治疗领域都有诸多阳性发现;然而SYMPLICITY HTN-3却一度让其跌入谷底。
2014年3月,SYMPLICITY HTN-3研究公布,结果显示,与假手术组对比,采用第一代Symplicity导管行RDN没有导致更显著的血压下降,自那以后RDN领域的研究经历了一段漫长的征途。尽管SYMPLICITY HTN-3设计严谨,但其执行中的缺陷和技术上的瓶颈,使其结论难以令人信服;其中术者经验不足和未实现完全神经阻断是其失败的两个重要原因。
二代四极Symplicity Spyral™导管和环形超声能源的Paradise®导管,分别使SPYRAL HTN-ON MED和RADIANCE-HTN SOLO研究获得成功,不仅让我们看到了经导管RDN的前景,也再次间接证明实现完全神经阻断是血压控制的关键,这也与早年外科RDN的疗效相吻合,也为我们探索高效消融指明了方向。然而,RADIANCE-HTN SOLO目前还只是得到短期结论,其长期疗效还有待观察;此外,该研究的获益人群是轻中度未服降压药的高血压患者,在口服降压药时代,其真实临床应用前景尚不乐观;而对于最需要非药物治疗的RH患者,经导管RDN的疗效还有待RADIANCE-HTN TRIO来回答。
研究人员从该试验中汲取了教训,并最终从假对照研究中获得了积极的结果,最开始是在一系列试点研究(如RADIANCE-HTN SOLO)中,然后是关键的SPYRAL HTN-OFFMED试验。
Tsioufis表示,这意味着除了改变生活方式和药物治疗外,抗高血压治疗有了第三大支柱。他说:“现代临床医生拥有RDN这项新颖的工具,可以更好地控制高血压。”他指出,关键性试验和假性对照试验均表明,该治疗方法既可对不使用任何药物的患者有效,也可作为服用多种药物且患有其他合并症的严重高血压患者的辅助手段。
Azizi补充说,RDN也减轻了患者的用药负担,“因此,我们希望这也将有助于改善药物依从性。”
Azizi继续说道,安全是一个至关重要的问题,特别是在考虑将侵入性手术用于心血管风险较低的患者中时。患者不应该接受会带来比自发风险更高的直接风险的手术。尽管在RDN早期,有一些与肾动脉导管插入术相关的并发症,例如动脉夹层,但在目前的实践中该手术变得更为安全。今天,如果我们研究不同的试验,就会看到短期和中期的并发症为零。
展望未来,Azizi表示仍然需要更好地确定哪些患者会对RDN有反应,因为RDN对患者血压的影响存在很大差异。以交感神经过度激活并伴有收缩期/舒张期高血压的年轻肥胖患者为RDN治疗目标可能是最合适的对象之一。
Tsioufis对此表示同意,但他表示,需要获得有关安全性和有效性以及手术标记开发的更多长期数据,术者可以使用这些数据来了解他们已经实现了完全神经支配。尽管如此,他说:“我们很高兴有更多方式可以改善血压控制,这应该是当务之急。”
Mahfoud表示,我们可以选择降低血压的方式,并能会做出更安全的选择。而且我们正在研究RDN新的适应症,包括在心律失常中的使用,如房颤,以及更多。我认为这是重要的一年,是我们在研究RDN方面所取得的重要一步。我们都应该持续关注。”
原始出处:
Lobo MD, Sharp ASP, Daemen J, Basile J, Weber MA, Scicli AP, McClure CK, Kirtane AJ.Changes in blood pressure after crossover to ultrasound renal denervation in patients initially treated with sham in the RADIANCE-HTN SOLO trial.EuroIntervention. 2021 Jul 9:EIJ-D-21-00295
Saxena M, Schmieder RE, Kirtane AJ, Mahfoud F, Daemen J, Basile J, Lurz P, Gosse P, Sanghvi K, Fisher NDL, Rump LC, Pathak A, Blankestijn PJ, Mathur A, Wang Y, Weber MA, Sharp ASP, Bloch MJ, Barman NC, Claude L, Song Y, Azizi M, Lobo MD. Predictors of blood pressure response to ultrasound renal denervation in the RADIANCE-HTN SOLO study.J Hum Hypertens. 2021 May 24. doi: 10.1038/s41371-021-00547-y
Azizi M, Daemen J, Lobo MD, Mahfoud F, Sharp ASP, Schmieder RE, Wang Y, Saxena M, Lurz P, Sayer J, Bloch MJ, Basile J, Weber MA, Rump LC, Levy T, Sapoval M, Sanghvi K, Rader F, Fisher NDL, Gosse P, Abraham J, Claude L, Barman NC, McClure CK, Liu Y, Kirtane AJ; RADIANCE-HTN Investigators. 12-Month Results From the Unblinded Phase of the RADIANCE-HTN SOLO Trial of Ultrasound Renal Denervation.JACC Cardiovasc Interv. 2020 Dec 28;13(24):2922-2933
Gosse P, Cremer A, Kirtane AJ, Lobo MD, Saxena M, Daemen J, Wang Y, Stegbauer J, Weber MA, Abraham J, Kario K, Bangalore S, Claude L, Liu Y, Azizi M. Ambulatory Blood Pressure Monitoring to Predict Response to Renal Denervation: A Post Hoc Analysis of the RADIANCE-HTN SOLO Study.Hypertension. 2021 Feb;77(2):529-536
Azizi M, Schmieder RE, Mahfoud F, Weber MA, Daemen J, Lobo MD, Sharp ASP, Bloch MJ, Basile J, Wang Y, Saxena M, Lurz P, Rader F, Sayer J, Fisher NDL, Fouassier D, Barman NC, Reeve-Stoffer H, McClure C, Kirtane AJ; RADIANCE-HTN Investigators. Six-Month Results of Treatment-Blinded Medication Titration for Hypertension Control Following Randomization to Endovascular Ultrasound Renal Denervation or a Sham Procedure in the RADIANCE-HTN SOLO Trial.Circulation. 2019 Mar 17. doi: 10.1161/CIRCULATIONAHA.119.040451
Azizi M, Schmieder RE, Mahfoud F, Weber MA, Daemen J, Davies J, Basile J, Kirtane AJ, Wang Y, Lobo MD, Saxena M, Feyz L, Rader F, Lurz P, Sayer J, Sapoval M, Levy T, Sanghvi K, Abraham J, Sharp ASP, Fisher NDL, Bloch MJ, Reeve-Stoffer H, Coleman L, Mullin C, Mauri L; RADIANCE-HTN Investigators.Endovascular ultrasound renal denervation to treat hypertension (RADIANCE-HTN SOLO): a multicentre, international, single-blind, randomised, sham-controlled trial.Lancet. 2018 Jun 9;391(10137):2335-2345
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#长期随访#
38
#DIA#
34
#结果公布#
0
#随访结果#
35
#肾动脉#
51
#消融#
30
#难治性#
23
#消融治疗#
31
不错,
55